Research Article
Role of Home Blood Pressure Monitoring in Overcoming Therapeutic Inertia and Improving Hypertension Control in Mexico

Hector Galvan Oseguera1, Martin Rosas Peralta2*, Jose Manuel Enciso Muñoz3 and ANCAM group for HBPM4
1Head of Heart Failure Department, UMAE Cardiology Hospital CMN SXXI, IMSS, Mexico2Head of Special Projects Area, Coordination of High Specialty Units, CUMAE-IMSS, Mexico
3Past President Asociación Nacional de Cardiólogos de México, (ANCAM), México
4Appendix, México
*Address for Correspondence: Dr. Martin Rosas Peralta, Head of Special Projects Area, Coordination of High Specialty Units, IMSS, Durango 289-1A Colonia Roma. Cuauhtémoc Delegation, 06700 México, Tel: 57261700; Email: [email protected]
Dates: Submitted: 18 January 2018; Approved: 08 February 2018; Published: 09 February 2018
How to cite this article: Oseguera HG, Peralta MR, Muñoz JME, ANCAM group for HBPM. Role of Home Blood Pressure Monitoring in Overcoming Therapeutic Inertia and Improving Hypertension Control in Mexico. Ann Clin Hypertens. 2018; 2: 017-023. DOI: 10.29328/journal.ach.1001007
Copyright License: © 2018 Oseguera HG, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hypertension; Domiciliary Blood Pressure monitoring; Ambulatory Blood Pressure; Mexico
Summary
Hypertension remains the most common modifiable cardiovascular risk factor, however, control of hypertension rates remain dismal. Home blood pressure (BP) monitoring has the potential to improve the control of hypertension. Home BP monitoring is now defended evenly for the evaluation and management of hypertension. This paper shows the experience of the National Association of Mexican Cardiologist in a group of patients with hypertension under drug treatment to evaluate the control in a real world clinical practice in Mexico. One hundred and fifty one patients were included. They were followed during two weeks with three home measurements at day (8:00, 14:00 and 20:00hr). An Ambulatory blood pressure of 24hr was performed at the middle of study. At the end of the study 36% (54/151) patients still uncontrolled by systolic blood pressure (>135 mmHg) and 31% by diastolic blood pressure similar results were detected by ambulatory blood pressure. During afternoon and night uncontrolled values were more common. Home blood pressure monitoring, results in a better form to detect uncontrolled patients and help clinical judgment to adjust pharmacological therapy. This practice should be recommended in Mexico.
Introduction
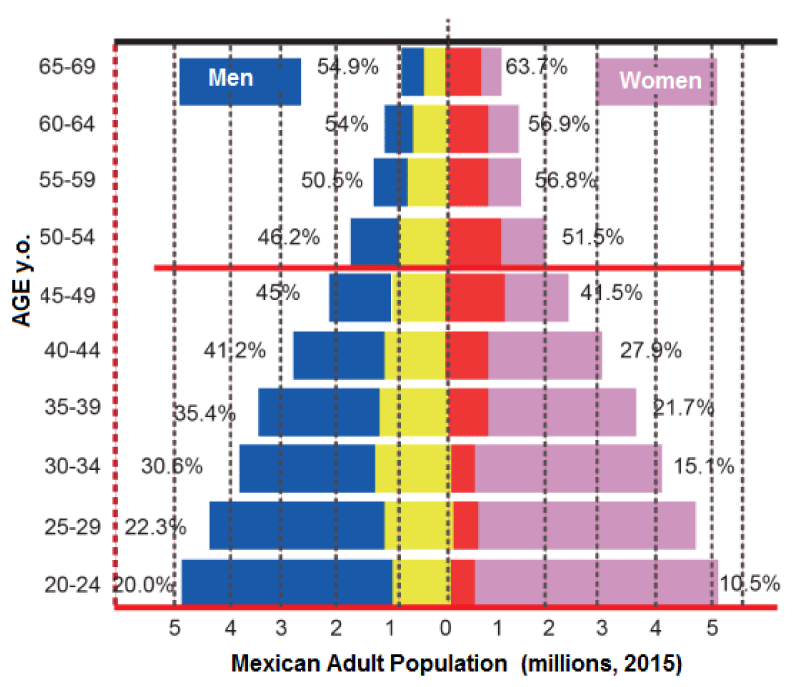
Hypertension remains the most common modifiable cardiovascular risk factor, yet hypertension control rates remain dismal. Home blood pressure (BP) monitoring has the potential to improve hypertension control [1]. Although, clinic blood pressure (BP) measurement still remains the cornerstone hypertension management, the broad availability of electronic BP measurement devices has led to their widespread adoption. Home BP monitoring is now uniformly advocated for the evaluation and management of hypertension [1,2]. This is so because BP control among treated hypertensives remains poor, and it is believed that home BP monitoring can improve hypertension control [1,2]. This improvement may be attributable to both better adherence with antihypertensive therapy and detection and treatment of masked hypertension. Further, in contrast to clinic BP measurement, which is associated with a white coat effect, home BP monitoring may reduce white coat effect and may obviate unnecessary therapy. In addition to improving hypertension control, home BP is superior to clinic BP in predicting cardiovascular prognosis and end-stage renal disease [3]. A previous meta-analysis [4] reported that home BP monitoring may improve hypertension control by only a small amount; however, even this small reduction was considered to be of public health importance. The purpose of this paper is to show our experience about hypertension control and to validate the magnitude of benefit in BP reduction with home BP monitoring. Further, and more important, it is to discover factors that may lead to improvement in BP control with this simple measurement technique. In Mexico the number of patients with hypertension with the cutoff point of 140/90 mmHg at 2015 was estimated in around 17 million in adults [5]. Its distribution by groups of age and gender is shown in figure 1.
Figure 1: Mexican adult population by groups of age and gender. The percentage of hypertensive patients is shown.
Methods
Identification and selection of patients
To identify patients with hypertension, a group of Cardiologists were invited to participate in this study. All of them received special training to include patients with hypertension and pharmacological therapy to evaluate home BP monitoring; they performed a structured questionnaire and register of daily BP measurements (morning, before breakfast ~8hr; middle day, before eat ~14hr; night, ~20hr). A digital Omron device Model: HEM7320 was used for BP monitoring. All patients were trained to use the device in adequate form and register the results in some leaves clip art for this. The study was developed for two weeks and a Monitoring Ambulatory Blood Pressure study was made in all patients at the middle of the study. Included patients were: aged ≥40 years, capable of informed consent, diagnosed with uncomplicated hypertension (without important Heart or Kidney injury secondary to hypertension), currently receiving at least one antihypertensive medication, regularly followed up for hypertension in the participating clinics, using their own upper arm-type HBPM machine to measure BP at home. Exclusion criteria were patients with any severe physical limitation, recent severe stroke, coexistence of terminal disease, heart failure, renal failure, primary hypertension.
Statistical analysis
Data are presented as the median, interquartile range. Statistical assessment was performed through one-way analysis of variance for repeated measures followed by Kruskal Wallis test with the IBM® SPSS Statistics® program for windows 21 version. Differences were considered statistically significant at p<0.05.
Results
One hundred and fifty one hypertensive patients were recruited between October 2016 and July 2017, 81 patients were men, mean age was 61±13 y.o. Mean systolic blood pressure was 137.5±19 mmHg; mean diastolic blood pressure was 83.5±12.5 mmHg.
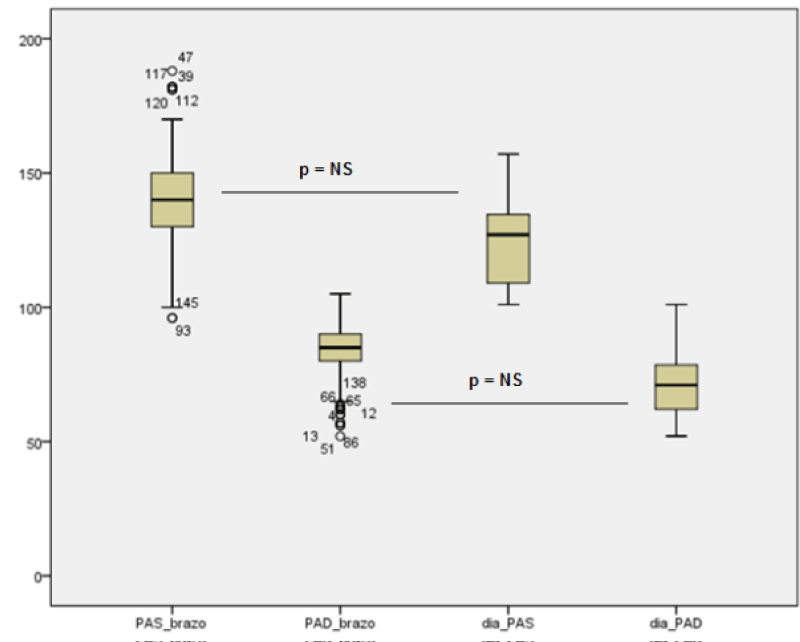
The dropout rate was 12.5% and 5.8% in the intervention and control group respectively. This translated to 105 completed in the intervention group and 113 in the control group. No significant difference was found in any of the baseline characteristics of the two groups (Figure 2). Over half had less than 3 years of experience in using HBPM machines.
Figure 2: Blood pressure monitoring, home versus ambulatory technique; there was not any statistical significance difference.
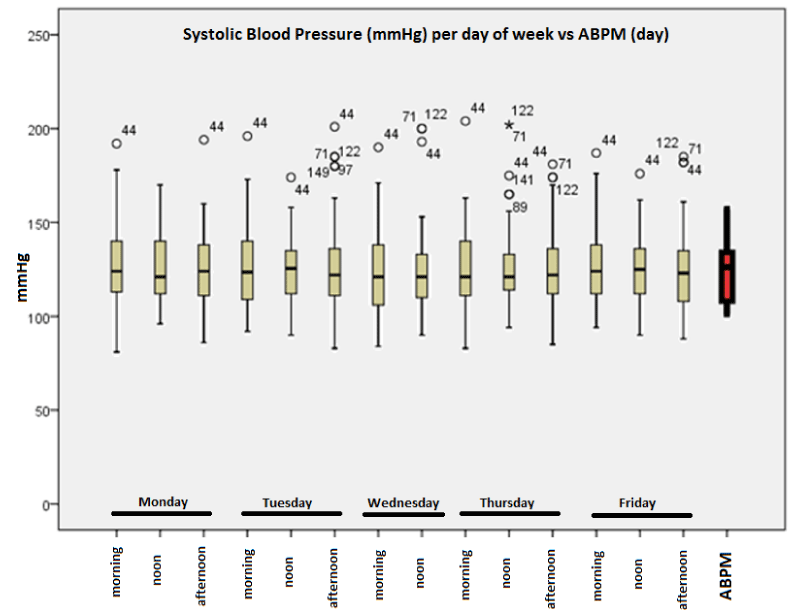
The mean SBP and DBP at baseline are shown in table 1. Both groups showed a decreasing trend in mean SBP and DBP from visits 1 to 3. Figure 3 shows the means BP within HBPM and ABPM respectively at one week, and the difference between both methods was no significant. Nevertheless the extreme values of some cases were detected only by HBPM. This was an advantage of this method.
Figure 3: Mean Values of SBP during one week (morning, noon, afternoon) and mean SBP (day) by ABPM. The 44, 71, 122 cases shown peaks of severe elevation.
| Table 1: Baseline Characteristics of study population (n=151). | |||
| Min | Max | Average±SD | |
| Age (years) | 29 | 88 | 61.3±12.8 |
| Height (mts) | 1.4 | 1.8 | 1.6±0.8 |
| Heart Rate (BPM) | 50 | 100 | 73±9 |
| Waist circumference (cm) | 65 | 139 | 95±13 |
| Systolic Blood Pressure (mmHg) | 98 | 170 | 137.5±19.3 |
| Diastolic Blood Pressure (mmHg) | 52 | 112 | 83.4±12.5 |
| Cholesterol (mg/dl) | 103 | 268 | 194.6±22.8 |
| Triglycerides (mg/dl) | 60 | 380 | 167±40 |
| HDL (mg/dl) | 22 | 65 | 49±17 |
| LDL (mg/dl) | 52 | 226 | 118±22.2 |
| Glucose (mg/dl) | 68 | 180 | 110±20 |
The reduction in DBP from start to finish study was significantly greater (an extra 5.84 mmHg, p=0.004) in the HBPM intervention group than in the baseline values. There was no statistically significant change in types and doses of anti-hypertensive medications used. Nevertheless the cases 44, 71 and 122 were detected to have hypertensive crisis and the pharmacological adjustment was able to reach the control of these patients.
Patient acceptability
Practices asked patients to record BP measurements using the ‘memory’ button on the machine and on a chart. Forty five patients (30%) had minimal problems with the memory button and a further five (4.5 %) had difficulty in reading the figures on the monitor. Nine (1.4%) had difficulty in entering figures on the chart. A total of 14 entries (the maximum number that the memory will store) were requested, and we found that chart records were more complete than those in the memory. Of chart entries, 133 (81%) patients made all 14 entries and only 11 (7.2%) made less than 10, whereas, of memory entries, 114 (76%) made 14 and 75 (49%) made less than 10. Using both machine and chart entries, 98% of patients produced 10 or more recordings.
A focus group highlighted the interest and enthusiasm that patients had for monitor use, their views on anxiety and BP variability, difficulties making recordings at work, and the importance of help from the practice nurses. One hundred and fifty (99%) patients said that cuff inflation was comfortable, and just one (0.9%) said that it was very uncomfortable or painful. Nine (6%) patients said that ABPM interfered with normal living; most of these having found that it was inconvenient to take a BP reading while at work.
Discussion and Recommendations
Home blood pressure monitoring (HBPM) overcomes many of the limitations of traditional office blood pressure (BP) measurement and is both cheaper and easier to perform than ambulatory BP monitoring. Monitors that use the oscillometric method are currently available that are accurate, reliable, easy to use, and relatively inexpensive [6-10]. An increasing number of patients are using them regularly to check their BP at home, but although this has been endorsed by national and international guidelines, detailed recommendations for their use have been lacking in Mexico. There is a rapidly growing literature [11-20], showing that measurements taken by patients at home are often lower than readings taken in the office and closer to the average BP recorded by 24-hour ambulatory monitors [21-26], which is the BP that best predicts cardiovascular risk. Because of the larger numbers of readings that can be taken by HBPM than in the office and the elimination of the white-coat effect (the increase of BP during an office visit), home readings are more reproducible than office readings and show better correlations with measures of target organ damage. In addition, prospective studies that have used multiple home readings to express the true BP have found that home BP predicts risk better than office BP (class IIa; level of evidence A) [27-32]. This call-to-action article makes the following recommendations: 1) It is recommended that HBPM should become a routine component of BP measurement in the majority of patients with known or suspected hypertension; 2) Patients should be advised to purchase oscillometric monitors that measure BP on the upper arm with an appropriate cuff size and that have been shown to be accurate according to standard international protocols. They should be shown how to use them by their healthcare providers; 3) Two to three readings should be taken while the subject is resting in the seated position, both in the morning and at night, over a period of 1 week. A total of ≥12 readings are recommended for making clinical decisions; 4) HBPM is indicated in patients with newly diagnosed or suspected hypertension, in whom it may distinguish between white-coat and sustained hypertension. If the results are equivocal, ambulatory BP monitoring may help to establish the diagnosis; 5) In patients with prehypertension, HBPM may be useful for detecting masked hypertension; 6) HBPM is recommended for evaluating the response to any type of antihypertensive treatment and may improve adherence; 7) The target HBPM goal for treatment is more clear for patients and definitely patients are involved in their healthcare. 7) In Mexico HBPM should be an important strategy to control hypertensive patients.
Appendix
ANCAM group for home blood pressure monitoring
Ciudad de México: Arriaga Nava Roberto, Castán Flores David Arturo, De la Cruz Rivera Armando Gilberto, Díaz Alvarez Juan José Ignacio, García Mayén Luis Fausto, Garduño Martínez Víctor Gregorio, Genis Zárate Jorge Héctor, González Trueba Esau, Luna Pérez David, Sánchez Pérez Rubén, Velarde Leyva Oscar Rodolfo, Monribot Velázquez Miguel Angel, Solis de la Rosa Federico, Sànchez Conejo Alma Rosa, Salgado Botello Hipòlito, Rodrìguez Martìnez René, Oliveros Ruiz Ma. Lucia, Montes Cruz Eliud Samuel, Martìnez Ortega Juan Ricardo, Guadarrama Arasi Josè Luis, Gonzàlez Delgadillo Silvia Susana, Cruz Alvarado Jaime Eduardo, Ancona Vadillo Ana Elena.
Monterrey: Contreras Morales Guillermo, Fong Ponce Manuel, Galván García José Eduardo, García Castillo Armando, García Martínez Rodrigo, Gonzalez Carrillo Luis Eduardo, González Salinas Aldo, Herrera Garza Eduardo Heberto, Ibarra Flores Marcos, Jáuregui Ruiz Oddir, Jiménez Torres Osvaldo, Lopez Zertuche Herminio, Martinez Dávila Sergio Ariel, Morales Salinas Feliciano Héctor Hernández Hernández José María, Sahagún Sánchez Guillermo.
Guadalajara: Álvarez López Humberto, Anguiano Torres Germán, Barrera Fausto Bolaños, Mario Briseño García Héctor Alberto, De la Torre Jiménez Narciso Ernesto, Fernández Váladez Eduardo, Hinojosa Pineda Pedro, Illescas Díaz Jesús Jaime, Merlin Elias, Morales Aceves Rubén, Peralta Heredia, Rogelio Rosa María Ríos, Robles López Héctor Genaro, Zavala Germán, De la Torre Jiménez Narciso Ernesto.
Puebla: Alcazar Casrín Emmanuel, Cardoso Alejandro, Izquierdo Vega Judith, Jiménez Hernández Jazmín, Jiménez Hernández Sandra, Julian Ramírez Denisse, López Hernández Emanuel, Mendoza Alfredo, Pierre Aristil Mitchel, Rivadeneira Torija Paola, Sánchez Pinal Juan, Soriano Orozco Laura.
Mérida: Barrera Bastillos Manuel, Farjat Ruiz Julio Iván, Jimenez Noh Joaquin Santaularia Tomas Miguel, Sierra Canto Gilberto, Wabi Dogre Carlos Humberto, Peralta Rosado Hilda R.
Acknowledgement
The Authors thank to Asociación Nacional de Cardiólogos de México its academic endorsement and to Omron Healthcare México its unconditional support to make this work.
References
- Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, et al. ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation and Management of High Blood Pressure in Adults. Hypertension. 2017. Ref.: https://goo.gl/qYWNMa
- Julius S. Home blood pressure monitoring: advantages and limitations. J Hypertens. 1991; 9: 41-46. Ref.: https://goo.gl/BgU1mu
- Burns-Cox CJ, Russel Rees J, Wilson RSE. Pilot study of home measurement of blood pressure by hypertensive patients. BMJ. 1975; 3: 80. Ref.: https://goo.gl/B5Mv7x
- Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta-analysis of randomised trials. BMJ. 2004; 329: 145. Ref.: https://goo.gl/giCB3W
- Encuesta Nacional de Salud y Nutrición de Medio Camino 2016. Mexico. Ref.: https://goo.gl/XuQKaF
- The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1997; 157: 2413-2446.
- Pickering TG, Devereux RB. Ambulatory blood pressure monitoring as a predictor of cardiovascular risk. Am Heart J. 1987; 114: 925-928. Ref.: https://goo.gl/xRVTvc
- O’Brien E, O’Malley K. Overdiagnosing hypertension. BMJ. 1988; 297: 1211-1212. Ref.: https://goo.gl/jLSMTC
- Haynes RB, Sackett DL, Gibson ES, Taylor DW, Hackett BC, et al. Improvement in medication compliance in uncontrolled hypertension. Lancet. 1976; 1: 1265-1268. Ref.: https://goo.gl/y4Z1Tf
- Soghikian K, Casper SM, Fireman BH, Hunkeler EM, Hurley LB, et al. Home blood pressure monitoring. Effect on use of medical services and medical care costs. Med Care. 1992; 30: 855-865. Ref.: https://goo.gl/oYCvgQ
- O’Brien E, Mee F, Atkins N, Thomas M. Evaluation of three devices for self-measurement of blood pressure according to the revised British Hypertension Society Protocol: The Omron HEM-705 CP, Philips HP5332 and Nissei DS-175. Blood Pressure Monitoring 1996; 1: 55-61.
- Sever P, Beevers G, Bulpitt C, Lever A, Ramsay L, et al. Management guidelines in essential hypertension: report of the second working party of the British Hypertension Society. BMJ. 1993; 306: 983-987. Ref.: https://goo.gl/buV7mg
- Mancia G, Sega R, Bravi C, De Vito G, Valagussa F, et al. Ambulatory blood pressure normality: results from the PAMELA study. J Hypertens. 1995; 13: 1377-1390. Ref.: https://goo.gl/zB6fBw
- Pickering TG. Blood pressure variability and ambulatory monitoring. Curr Opin Nephrol Hypertens. 1993; 2: 380-385. Ref.: https://goo.gl/8jSGgD
- Brueren MM, Schouten HJ, de Leeuw PW, van Montfrans GA, van Ree JW. A series of self-measurements by the patient is a reliable alternative to ambulatory blood pressure measurement. Br J Gen Pract. 1998; 48: 1585-1589. Ref.: https://goo.gl/HqESEn
- HMSO. Morbidity Statistics from General Practice 1991-1992. London: Stationery Office. 1995.
- Sever P. How well are we managing blood pressure? Lancet. 1994; 344: 1019-1020. Ref.: https://goo.gl/3Jbhp9
- Aylett M, Creighton P, Jachuck S, Newrick D, Evans A. Blood pressure control of drug treated hypertension in 18 general practices. J Hum Hypertens. 1996; 10: 547-550. Ref.: https://goo.gl/JKgQep
- Mashru M, Lant A. Interpractice audit of diagnosis and management of hypertension in primary care: educational intervention and review of medical records. BMJ. 1997; 314: 942-946. Ref.: https://goo.gl/x6riwF
- Prasad N, Isles C. Ambulatory blood pressure monitoring: a guide for general practitioners. BMJ. 1996; 313: 1535-1541. Ref.: https://goo.gl/V5R6um
- Sega C, Casana G, Pagani R, Bravi C, Vito G De, et al. Ambulatory and home blood pressure reference values: the PAMELA Study. J Hypertens. 1993; 11: 481. Ref.: https://goo.gl/L44wus
- Aylett MJ. The use of home blood pressure measurements to diagnose white coat hypertension in general practice. J Hum Hypertens. 1996; 10: 17-20. Ref.: https://goo.gl/8e7zR1
- McGrath BP. Is white-coat hypertension innocent? Lancet. 1996; 348: 630. Ref.: https://goo.gl/3PnRmw
- Mancia G, Zanchetti A. White-coat hypertension: misnomers, misconceptions and misunderstandings. What should we do next? J Hypertens. 1996; 14: 1049-1052. Ref.: https://goo.gl/soM9Ag
- Spence JD, Lacourciere Y, Guibert R, et al. Is it safe to withhold treatment in white coat hypertension? J Hypertens. 1998; 16: 27055-27055.
- Hall CL, Higgs CMB, Notarianni L. Value of patient recorded home blood pressure series in distinguishing sustained from office hypertension: effects on diagnosis and treatment of mild hypertension. J Hum Hypertens. 1990; 4: 9-13. Ref.: https://goo.gl/meky8h
- Harrison DW, Crews WD Jr. The Takeda Model UA-751 blood pressure and pulse rate monitor. Biomed Inst Tech. 1992; 26: 325-327. Ref.: https://goo.gl/Wodhce
- Gaudemaris. Home blood pressure: variability, comparison with office readings and proposal for reference values. J Hypertens. 1994; 12: 831-838. Ref.: https://goo.gl/MKgujS
- Chatellier G, Dutrey-Dupagne C, Vaur L, Zannad F, Genès N, et al. Home blood pressure measurement in general practice (the SMART study). Am J Hypertens. 1996; 9: 644-652. Ref.: https://goo.gl/487FfT
- Celis H, De Cort P, Fagard R, Thijs L, Staessen JA. For how many days should blood pressure be measured at home in older patients before steady levels are obtained? J Hum Hypertens. 1997; 11: 673-677. Ref.: https://goo.gl/5ouFsx
- O’Brien E. Review: A century of confusion; which bladder for accurate blood pressure measurement? J Hum Hypertens. 1996; 10: 565-572. Ref.: https://goo.gl/8MpD49
- Donner-Banzhoff N, Chan Y, Szalai JP, Hilditch J. ‘Home hypertension’: exploring the inverse white coat response. Br J Gen Pract. 1998; 48: 1491-1495. Ref.: https://goo.gl/yxCT9V