Review Article
What is new in Hypertension of Mexico 2018?
-Impact of the new classification of high blood pressure in adults from American College of Cardiology/American Heart Association (ACC/AHA)

Martin Rosas-Peralta1, Gabriela Borrayo-Sánchez2*, Janaí Santiago-López3, Erick Ramirez Árias4, Rosalba García Méndez5, Victor Hugo Borja-Aburto6, Ana Carolina Sepúlveda-Vildósola7 and José de Jesús Arriaga-Dávila8
1Head of Special Projects Area, Coordination of High Specialty Units; CUMAE-IMSS, Mexico2Technical Coordinator for prevention and treatment of cardiovascular diseases, IMSS Mexico
3Special Projects Area, Coordination of High Specialty Units; CUMAE-IMSS, Mexico
4Head of Emergency Room, Cardiology Hospital, National Medical Center SXXI, IMSS Mexico
5Research in Health, Cardiology Hospital, National Medical SXXI, IMSS Mexico
6Head of Primary Health Care Unit, IMSS México
7Head of Investigation and Education and Political Health Unit, IMSS México
8Head of Medical Benefits of IMSS, Mexico
*Address for Correspondence: Dra. Gabriela Borrayo-Sánchez. Comisionada del Programa A Todo Corazón-Código Infarto, IMSS México. Avenida Cuauhtémoc 330 Doctores. 0670 CDMX, Email: [email protected]
Dates: Submitted: 20 February 2018; Approved: 06 March 2018; Published: 07 March 2018
How to cite this article: Rosas-Peralta M, Borrayo-Sánchez G, Santiago-López J, Árias ER, Méndez RG, et al. What is new in Hypertension of Mexico 2018? -Impact of the new classification of high blood pressure in adults from American College of Cardiology/American Heart Association (ACC/AHA). Ann Clin Hypertens. 2018; 2: 024-030. DOI: 10.29328/journal.ach.1001008
Copyright License: © 2018 Rosas-Peralta M, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hypertension; Cardiovascular risk; Epidemiology; Prevention; IMSS; Mexico
Abstract
The new report of American College of Cardiology/American Heart Association task force on Clinical Practice Guidelines for High Blood Pressure in Adults was published online ahead of print November 13, 2017. The new American recommendation was focused on the criteria to define Hypertension. 130/80 mmHg or more is now considered as the new cut off point to define Hypertension. It is not new if we consider cumulative evidence in the las two decades has been broken the idea to consider 140/90 mmHg as the point to start medical actions. Thus, in México with current ACC/AHA definition it is estimated today around 48 million of adult hypertensive population. In the Mexican Institute of Social Security (IMSS) several strategies has been developed to improve prevention as the key action to confront non communicable chronic disease including hypertension. This updated guideline from ACC/AHA is an extraordinary opportunity to reinforce our preventive programs to high blood pressure control. In this brief report we analyze the epidemiological situation in Mexico and its possible consequences of the new criteria for hypertension diagnosis. The main current strategies that are applied into the IMSS to confront cardiovascular risk factors are directed to prevention. The IMSS is prepared to attend situations as the change of criteria diagnoses in Hypertension and new preventive models are in progression.
Introduction
In Mexico the prevalence of arterial hypertension in adults aged over 20 years old had been around 30%±2% according to the national surveys of health in the year 2000, 2006, and 2012[1,2]. However, the “half way” national health survey from 2016 [3] reported a prevalence of 25.5% and this drastic decrease was explained as a consequence of methodological aspects. This would have no apparent significance; however, we need keep in mind that it is the most common cardiovascular risk factor associated with coronary artery disease and cardiovascular death.
The new report of American College of Cardiology/American Heart Association task force on Clinical Practice Guidelines for High Blood Pressure in Adults was published online ahead of print November 13, 2017 [4]. The new American recommendation was focused on the criteria to define Hypertension. 130/80 mmHg or more is now considered as the new cut off point to define Hypertension. This dramatic feature of the new guidelines will likely influence the management of hypertension globally but especially in countries such as Mexico already facing an enormous public health challenge (with the previous definition of hypertension ≥140/90 mm Hg). The high incidence of hypertension in Mexico (a result of lower thresholds), however, should not be dismissed as absurd or impractical. Rather, it is a clarion call to reduce the dreadful consequences of chronic disease burden driven by elevated BP levels. Time has come (but not run out) to implement effective public health policy on a war footing for accurate measurement of BP and effective treatment of hypertension of any degree. Nevertheless they claim that this classification gives more opportunity to not pharmacological preventive medicine.
It is known that the cardiovascular risk starts from 120/80 mmHg. Nonetheless, high blood pressure is a continuous process and its cut off points to classify and make diagnosis of hypertension should be taken in account very carefully. In other words, a patient with diabetes and blood pressure of 135/83 with evidence of injury to white organ (i.e. microalbuminuria) must be considered to pharmacological therapy additionally to life style changes. On the other side a patient with the same blood pressure level but without evidence of injury to white organ and only overweight, changes in weight and life style could be enough.
The ACC and AHA sponsor the development and publication of guidelines on November 2017. Guidelines are official policy of the ACC and AHA and they have added a new classification of Hypertension (Table 1).
| Table 1: New Classification of Hypertension (AHA/ACC November 2017). | |
| Normal: | Less than 120/80 mm Hg |
| Elevated: | 120-129/less than 80 mm Hg |
| Stage 1 Hypertension: | 130-139/80-89 mm Hg |
| Stage 2 Hypertension: | At least 140/90 mm Hg |
| Hypertensive crisis: | Over 180/120 mg Hg |
Thus, the updated guideline classifies hypertension as a BP reading of 130/80 mmHg or higher. As a consequence the absolute number in millions of patients with a diagnosis of high blood pressure increased exponentially. We present in this brief report the epidemiological situation of hypertension in Mexico, and the current strategies to confront this pandemic.
National health survey (ENSANUT 2012)
In Mexico the prevalence in 2012 was from 31.5% (95% CI 29.8 33.1), (figure to the majority of Latin American countries) and is highest in adults with obesity ((42.3%) 95% CI 39.4-45.3) in adults with normal (BMI) body mass index ((18.5%) 95% CI 16.2-21.0), and in adults with diabetes ((65.6%) 95% CI 60.3-70.7) that without this disease (27.6%, 95% CI 29.2-26.1). In addition, during the 2012 ENSANUT observed that 100% of hypertensive adults 47.3% unaware from hypertension.
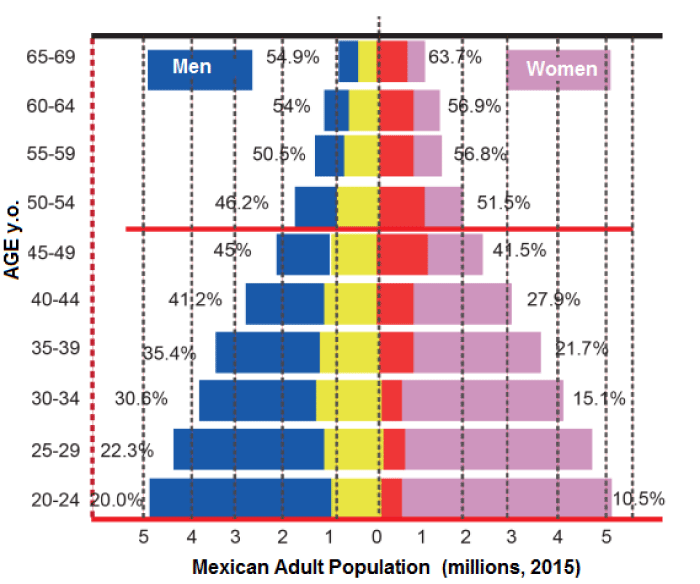
The trend of hypertension in the last six years (2006-2012) has remained stable both in men (32.4 vs 32.3%) and women (31.1 vs 30.7%) and the proportion of individuals with prior diagnosis did not increase in the previous six years. Differences between the prevalence of the major and minor age groups, e.g. in 2012 are also similar in its distribution of the prevalence of hypertension was 4.6 times lower in the Group of 20 to 29 years of age (p<0.05) than in the Group of 70 to 79 years (Figure 1).
Figure 1: Hypertensive Adult Population in Mexico (2015) with cutoff point of 140/90 mmHg; the percentage into each age group by sex are illustrated.
The prevalence of hypertension varied according to regions, towns and socioeconomic level (SEL). Thus, a prevalence significantly higher (p<0.05) in the northern region of the country (36.4%) was detected compared with the South (28.5%), in urban localities (31.9%) and in rural areas (29.9%). In other words, the hypertension prevalence needs to be considered according with geographical and sociological conditions. In addition, the individual characteristics such as age, associated comorbidities, weight, sex, genetic and education must be keep in mind. http://ensanut.insp.mx/doctos/analiticos/HypertensionArterialAdultos.pdf (2012). Around 17 million of hypertensive patients were estimated in 2015, see figure 1.
Half-way National health survey (HW-ENSANUT 2016)
A national probabilistic, conglomerated, stratified and cluster with regional and urban and rural representation health survey was performed. 9,474 homes were explored; 29,795 individuals of the following age groups were selected at random: 5-11 years (school age), 12-19 years (adolescents) and 20 and more years (adults). The sampling framework of primary units in urban areas was the list of BGA (Basic Geo-statistics Areas) built by the INEGI (National Institute of geography and statistics) 2010 census. The rising period May to October 2016.
High Blood Pressure
In the HW-ENSANUT 2016, the blood pressure measurement was performed using a digital device (Omron HEM-907 XL). In the other hand, the 2012 ENSANUT survey the blood pressure measurement was performed using mercury device. The same protocol was used in both surveys and procedures recommended by the American Heart Association [2]. Information analysis only considered valid data all those values of systolic blood pressure (TAS) greater than 80 mmHg and voltage greater than 50 mmHg diastolic blood pressures (DBP). The classification used for categorizing the blood pressure was described in the national report for the diagnosis of Arterial high blood pressure (JNC 8). It was classified as Normotensive adults with TAS<140 mmHg and TAD<90 mmHg; and as hypertensive adults who reported having previously received a medical diagnosis of high blood pressure (hypertension), or had figures of TAS≥140 mmHg or TAD≥90 mmHg.
Adults with hypertension were considered as controlled when systolic was <140 mmHg and diastolic was <90 mmHg. It should be noted that this report was presented according to adjusted prevalence by findings, and therefore these prevalence differ from those reported in publications where the adjustment to national survey was not made. This is the case of HW-ENSANUT 2016 where the prevalence of hypertension was reported in 25.5%, 40.0% of them had been unaware of hypertension diagnosis and only the 58.7% of adults with prior diagnosis were found in adequate control (< 140/90 mmHg). The diagnosis of this disease tends to be higher in women than in men (70.5 vs 48.6%) and decreased 7.8% from 2012 to 2016. Although this prevalence has remained virtually unchanged between 2012 and 2016, because of the consequences that causes on the health of the population, the efforts of the health system should step up for improving the prevention and control of who and the suffers from.
Impact of new ACC/AHA criteria [4] for diagnosis of Hypertension in Mexico
In Mexico for example at the middle of 2017 exists around ~128 million people, 65% of them (76 million) corresponds to population aged over 20 years old. Pre-hypertension or also called borderline blood pressure was considered in previous JNC-8 report and its prevalence was informed around 25-30% in the adult population. In Mexico, the prevalence of pre hypertension was informed in 2015 to be 37.5% (95% confidence interval (CI): 36.0–39.0): 46.7% were men (95% CI: 44.1-49.4) and 33.2% (95% CI: 31.5–5.0) were women [5]. This is a dramatic national situation because of 37% of prehypertension in Mexico represents around 30.9 million adult population. In addition with a prevalence estimated in 30% around 22.8 million would be within the diagnosis of hypertension with criteria of 140/90 mmHg, but with the new criteria of the AHA, as we mentioned before, the population with hypertension is at least twice. This is a real epidemiological alert that will require new strategies to confront it. Therefore, In other words, we need programs to prevention and treatment that should be established to around 53 million of adults in Mexico. It reinforce epidemiological alert of an old problem with new diagnostic-therapeutic challenges.
However, the problem does not end with the new number of patients with a diagnosis of hypertension. It must take into account that the rate of patients detected, treated and controlled with the previous breakpoint of 140/90 mmHg was low and not enough, therefore with the new cutoff point of 130/80 mmHg, the percentage of patients with hypertension controlled is reduced even more. While the focus of ACC/AHA [4] seeks to address with greater emphasis preventive and non-pharmacological actions to treat hypertension implications real in countries like Mexico represent one major health challenge it publishes. The need to establish a position is clear and necessary.
Current Actions
The epidemiological transition of diseases in Mexico is recognized since the end of the last century. National health surveys, allowed the Government of Mexico to establish health policies directed specifically to confront this new pandemic. At the beginning of the new century came out of integrated programs of health now called PREVENIMSS. The integrated health programs, recognized as a strategy for the provision of services, which had as their general purpose the provision of systematic and orderly of related actions such as health promotion, nutrition surveillance, prevention, detection and control of diseases and reproductive health; stimulating in this way the culture of self-care. Today the results of this strategy are very relevant. The population served (PA) with respect to the target population went from 45 percent in 2008 to 65 percent in 2016. In this way, emphasizes the continuous rise in absolute numbers of the PA which grew at 80.1 percent, in particular for the advancement of the goals of the global indicator of comprehensive care PREVENIMSS between 2008 and 2016. Moreover, the budget of the programed to 2012 prices grew a 27.7% between 2011 and 2016.
Despite the improvement in timely detection of chronic diseases, the great challenge is to achieve figures even higher for patients treated and controlled to avoid the generation of late complications such as heart attack of myocardium and brain, as well as arterial disease peripheral, kidney failure and blindness secondary to hypertensive and diabetic retinopathy. Online training systems have enabled to achieve greater coverage and seek to standardize the knowledge and direct actions in the operating field.
Constant alert even deficit-control ailments such as hypertension, diabetes, obesity, Dyslipidemia and smoking gender the search for alternatives to confront two fronts at the same time: i) timely detection and risk stratification (adequate (risk calculator) and ii) increase the percentage of long-term cardiovascular risk factors monitoring and control [6-14]. It recently published a special supplement focused on the national consensus of arterial hypertension in Mexico and specific clinic situation [17-20].
Preventive Model
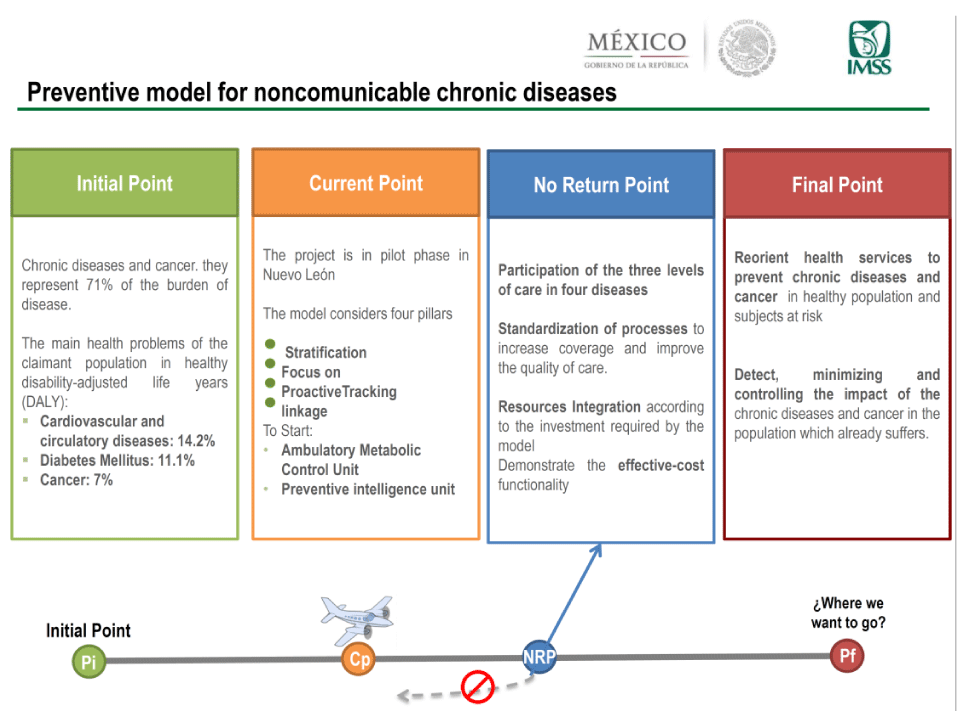
The Mexican of the Social Security Institute (IMSS), adjusted its model of care of the curative to preventive, to deal with the growth of the four major chronic degenerative diseases (diabetes, cardiovascular ailments, breast and prostate cancer) that are the main causes of death in the country [21,22]. The new model is to deploy medical brigades to workplaces and create new clinics in specialized medicine, supported by an intelligence unit that will focus a follow-up, electronic board and custom data in time detected the potential risks that present beneficiaries about these diseases. The development of centers of ambulatory metabolic control with artificial intelligence units, represent a breakthrough of the IMSS and has been established in this administration the point of no return figure 2.
Chiquiti-IMSS & SI Program [23,24]
The Mexican Institute of social security aware that changes in eating habits and life style have to begin from an early age actions in this regard have been deployed. Thus there are educational programs of health in child care and guidance in balanced nutrition as a preventive measure of obesity and chronic diseases. Recently also established a special education program for preschoolers that includes body health and knowledge of the cardiovascular system as well as handling of emotions, this pilot program will be implemented in 2018.
Future
Prevention is angular piece in the care of the healthy patient at risk of developing the disease and secondary way to prevent complications of the already carriers of the same. The systemic arterial hypertension as one of the main factors of cardiovascular risk is not something new to the IMSS. Be aware that disease is a continuous and that their risk starts from 120/80 mmHg, however should individualize each case, Stratify properly and complete your cardiovascular risk and establish preventive measures as a first step. The change in eating habits and exercise must be set in all hypertensive patients unless this contraindicated. The generation of cohorts in follow-up to know the impact of pharmacological, preventive measures and quality of life in the new models are the challenge that will dictate the health policy of the institution more in health in Latin America.
Acknowledgement
The authors want to thank to IMSS foundation, particularly to its general director, Lic. Patricia Guerra by her unconditional support and endorsement in the elaboration and diffusion of this work.
References
- Velázquez Monroy O, Rosas Peralta M, Lara Esqueda A, Pastelín Hernández G, Attie F, et al. Hipertensión Arterial en México: Resultados de la ENSA 2000. Arch Cardiol Mex. 2002; 72: 71-84. Ref.: https://goo.gl/XRK1bT
- ENSANUT 2012. Hipertensión arterial en adultos mexicanos: importancia de mejorar el diagnóstico oportuno y el control. Ref.: https://goo.gl/t3rFU1
- Encuesta Nacional de Salud y Nutrición de Medio Camino 2016. Ref.: https://goo.gl/LnNtKh
- Whelton PK, Carey RM, Aronow WS, Casey DE Jr, Collins KJ, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol. Hypertension. 2017; 1097: 41519-41521. Ref.: https://goo.gl/iM2eix
- Rodríguez-Ramírez M, Simental-Mendía LE, González-Ortiz M, Martínez-Abundis E, Madero A, et al. Prevalence of Prehypertension in Mexico and Its Association with Hypomagnesemia. Am J Hypertension. 2015; 28: 1024-1030. Ref.: https://goo.gl/hyR1zX
- Jaffe MG, Young JD. The Kaiser Permanente Northern California story: improving hypertension control from 44% to 90% in 13 years (2000 to 2013). J Clin Hypertens. 2016; 18: 260-261. Ref.: https://goo.gl/KifGHc
- Smith SC Jr, Benjamin EJ, Bonow RO, Lynne TB, Mark AC, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. J Am Coll Cardiol. 2011; 58: 2432-2446. Ref.: https://goo.gl/tHwFFo
- Standards of Medical Care in Diabetes-2016: Summary of Revisions. Diabetes Care. 2016; 39: 4-5. Ref.: https://goo.gl/xwCdy9
- Hysong SJ, Simpson K, Pietz K, SoRelle R, Broussard Smitham K, et al. Financial incentives and physician commitment to guideline-recommended hypertension management. Am J Manag Care. 2012; 18: 378-391. Ref.: https://goo.gl/WN844V
- Petersen LA, Simpson K, Pietz K, Urech TH, Hysong SJ, et al. Effects of individual physician-level and practice-level financial incentives on hypertension care: a randomized trial. JAMA. 2013; 310: 1042-1050. Ref.: https://goo.gl/umG3QM
- Karunaratne K, Stevens P, Irving J, Hobbs H, Kilbride H, et al. The impact of pay for performance on the control of blood pressure in people with chronic kidney disease stage 3-5. Nephrol Dial Transplant. 2013; 28: 2107-2116. Ref.: https://goo.gl/pobq5C
- Maimaris W, Paty J, Perel P, Legido-Quigley H, Balabanova D, et al. The influence of health systems on hypertension awareness, treatment, and control: a systematic literature review. PLoS Med. 2013; 10: 1001490. Ref.: https://goo.gl/cGKqTS
- Center for Medicare and Medicaid Services. Million Hearts: Cardiovascular Disease Risk Reduction Model. 2016. Ref.: https://goo.gl/DjFpGm
- Walsh JM, McDonald KM, Shojania KG, Sundaram V, Nayak S, et al. Quality improvement strategies for hypertension management: a systematic review. Med Care. 2006; 44: 646-657. Ref.: https://goo.gl/Qm58er
- Jaffe MG, Lee GA, Young JD, Sidney S, Go AS. Improved blood pressure control associated with a large-scale hypertension program. JAMA. 2013; 310: 699-705. Ref.: https://goo.gl/Crh8tF
- Rosas-Peralta M, Borrayo-Sánchez G, Madrid-Miller A, Ramírez-Arias E, Pérez-Rodríguez G. Hipertensión arterial sistémica en el adulto mayor. Recomendaciones para la práctica clínica. Rev Med Inst Mex Seg Soc. 2016; 54: 75-77. Ref.: https://goo.gl/p761qx
- Martín Rosas-Peralta, Silvia Palomo-Piñón, Gabriela Borrayo-Sánchez, Alejandra Madrid-Miller, Eduardo Almeida-Gutiérrez, et al. Consenso de Hipertensión Arterial Sistémica en México. Rev Med Inst Mex Seguro Soc. 2016; 54: 6-51. Ref.: https://goo.gl/Cht2F7
- Rosas-Peralta M, Borrayo-Sánchez G, Ramírez-Arias E, Madrid-Miller A, Perez-Rodriguez G. Complicaciones cardiovasculares de la crisis hipertensiva. Rev Med Inst Mex Seguro Soc. 2016; 54: 67-74. Ref.: https://goo.gl/MeyKfx
- Rosas-PeraltaM, Medina-Concebida L, Borrayo-Sánchez G, Madrid-Miller A, Ramírez-Arias E, et al. Hipertensión arterial sistémica en el niño y adolescente. Rev Med Inst Mex Seguro Soc. 2016; 54: 52-66. Ref.: https://goo.gl/kFDEv7
- Borja Aburto VH, Salud Pública. Salud pública, Ed. Alfil. 1a. Edición. 2013.
- CHKT en línea. PREVENIMSS. Ref.: https://goo.gl/WdyHpH
- Castañeda-Sánchez O, Ruelas-Oliveros G. Efecto de una intervención educativa en preescolares con factores de riesgo cardiovascular en Ciudad Obregón, Sonora. Aten Fam. 2015; 22: 77-81. Ref.: https://goo.gl/LZnHQJ
- ChiquitIMSS, Programa de salud del niño de 5 a 9 años. 2014. Ref.: https://goo.gl/j7zdtB
- Peñalvo JL, Santos-Beneit G, Sotos-Prieto M, et al. The SI! Program for Cardiovascular Health Promotion in Early Childhood. JACC. 2015; 66: 1525-1536. Ref.: https://goo.gl/kqVPf7