Review Article
Role of the Kidneys in the Regulation of Intra-and Extra-Renal Blood Pressure

Seriki A Samue1*, Adebayo O Francis1 and Odetola O Anthony2
1Department of Human Physiology, College of Medicine, Bingham University, Karu, Nigeria2Department of Human Physiology, Faculty of Medicine, Nnamdi Azikiwe University, Awka, Nigeria
*Address for Correspondence: Seriki A. Samuel, Department of Human Physiology, College of Medicine, Bingham University, Karu, Nigeria, Tel: +2348036041121; Email: [email protected]
Dates: Submitted: 05 July 2018; Approved: 16 July 2018; Published: 17 July 2018
How to cite this article: Samuel SA, Francis AO, Anthony OO. Role of the Kidneys in the Regulation of Intra- and Extra-Renal Blood Pressure. Ann Clin Hypertens. 2018; 2: 048-058. DOI: 10.29328/journal.ach.1001011
Copyright License: © 2018 Samuel SA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Hypertension; Renin Angiotensin System; Natriuresis; Sodium balance homeostasis
Abstract
Hypertension is one of the most common chronic diseases of human, affecting more than one billion people worldwide. When it becomes chronic, hypertension leaves behind cardiac hypertrophy, heart failure, stroke, and kidney disease, resulting in substantial morbidity and mortality. Treatments that effectively reduce blood pressure can prevent these complications. Abnormalities in the production of urine by the kidneys have been implicated in increased vascular resistance, leading to high blood pressure and increased cardiac mass. By matching urinary excretion of salt and water with dietary intake, balance is usually attained, thereby maintaining a constant extracellular fluid volume and blood pressure. Based on the capacity for the kidney to excrete sodium, this blood pressure-altering mechanism should have sufficient advantage to limit intravascular volume and consequently lower blood pressure in response to a range of stimuli from elevated heart rate to increase peripheral vascular resistance. A major determinant of the level of intra- and extra- renal blood pressure is therefore sodium handling, and it is controlled by complex physiological mechanism by hormones, inflammatory mediators, and the sympathetic nervous system. Homoeostasis and favourable influence sodium balance are a basic mechanism of efficacy for diuretics and dietary sodium restriction in hypertension. Renin Angiotensin System (RAS) inhibitors, vasodilators, and β-blockers work to facilitate pressure-natriuresis. Also, WNK signaling pathways, soluble inflammatory mediators, and pathways regulating extra-renal sodium disposition may be the focus towards elimination of sodium and reducing blood pressure in hypertension.
Introduction
That the kidney plays a role in hypertension is a knowledge that dates back almost 200 years some a researcher postulated that abnormalities in urine production by the kidney altered blood in such a way that tends to increase vascular resistance, leading to high blood pressure and increased cardiac mass. Many years later, Harry Goldblatt also induced malignant hypertension in dogs by obstructing one of the renal arteries [1]. Arthur Guyton and colleagues also advanced a hypothesis suggesting that the kidney governs the level of blood pressure by regulating extracellular fluid volume in 1970. They argued that balance is normally achieved by matching urinary excretion of salt and water with dietary intake, thereby maintaining a constant extracellular fluid volume and blood pressure [2]. They explained that when blood pressure increases for any reason, renal perfusion pressure also increases thereby enhancing sodium and water excretion, which Guyton referred to as pressure-natriuresis.
Based on the capacity for the kidney to excrete sodium, this blood pressure-altering mechanism should have sufficient advantage to limit intravascular volume and consequently lower blood pressure in response to a range of stimuli from elevated heart rate to increase peripheral vascular resistance [2]. Furthermore, a permissive modification of the pressure-natriuresis response has been predictably required to perpetuate a chronic elevation in intra-arterial pressure, whereby the equilibrium point for salt and water excretion is shifted to a higher level of arterial blood pressure [3]. Also, a series of kidney cross-transplantation studies have supported a key role for intrinsic functions of the kidney in the pathogenesis of hypertension [4]. Genetically, compatible donor and recipient strains were used to circumvent rejection, with both native kidneys removed such that the full extent of excretory function is provided by the transplanted kidney [4].
Likewise, studies in spontaneously hypertensive rats and Milan hypertensive rats recapitulated these findings. The same principle seems to also hold true in humans where resistant hypertension can be alleviated after successful kidney transplantation [5]. Collectively, these studies point to the fact that a defect in sodium excretion by the kidney confers susceptibility to elevated blood pressure.
Blood pressure and hypertension
Hypertension is one of the most common chronic diseases of human, affecting more than one billion people worldwide [6]. Although elevated blood pressure does not typically cause overt symptoms, the consequences of chronic hypertension, including cardiac hypertrophy, heart failure, stroke, and kidney disease, are responsible for substantial morbidity and mortality. Treatments that effectively reduce blood pressure can prevent these complications [7]. However, in recent times, blood pressures were reduced to target levels in less than 50% of patients receiving hypertension treatment, and this rate was under 40% in individuals who also had chronic kidney disease (CKD) [8].
The reasons for these poor outcomes include health services issues around processes of care, compliance, and patient education. Moreover, the precise cause of hypertension is not apparent in the vast majority of patients with hypertension. Limitations in understanding of hypertension pathogenesis in individual patients are an obstacle to applying individualized approaches for prevention and treatment and to identifying new, specific therapies.
The kidneys and their influence on blood pressure
The kidneys play a central role in the regulation of arterial blood pressure. A large body of experimental and physiological evidence indicates that renal control of extracellular volume and renal perfusion pressure are closely involved in maintaining the arterial circulation and blood pressure. Renal artery perfusion pressure directly regulates sodium excretion; a process known as pressure natriuresis, and influences the activity of various vasoactive systems such as the renin–angiotensin–aldosterone (RAS) system [9]. Along with vessel morphology, blood viscosity is one of the key factors influencing resistance and hence blood pressure. A key modulator of blood viscosity is the renin-angiotensin system (RAS) or the renin-angiotensin-aldosterone system (RAAS), a hormone system that regulates blood pressure and water balance.
The blood pressure in the body depends upon:
• The force by which the heart pumps out blood from the ventricles of the heart - and this is dependent on how much the heart muscle gets stretched by the inflowing blood into the ventricles.
• The degree to which the arteries and arterioles constrict-- increases the resistance to blood flow, thus requiring a higher blood pressure.
• The volume of blood circulating round the body; if the volume is high, the ventricles get more filled, and the heart muscle gets more stretched.
The kidney influences blood pressure by:
• Causing the arteries and veins to constrict
• Increasing the circulating blood volume
Specialized cells called macula densa are located in a portion of the distal tubule located near and in the wall of the afferent arteriole. These cells sense the Na in the filtrate, while the arterial cells (juxtaglomerular cells) sense the blood pressure. When the blood pressure drops, the amount of filtered Na also drops. The arterial cells sense the drop in blood pressure, and the decrease in Na concentration is relayed to them by the macula densa cells. The juxtaglomerular cells then release an enzyme called renin.
Renin converts angiotensinogen (a peptide, or amino acid derivative) into angiotensin-1. Angiotensin-1 is thereafter converted to angiotensin-2 by an angiotensin-converting enzyme (ACE), found in the lungs. Angiotensin-2 causes blood vessels to contract -- the increased blood vessel constrictions elevate the blood pressure. When the volume of blood is low, arterial cells in the kidneys secrete renin directly into circulation. Plasma renin then carries out the conversion of angiotensinogen released by the liver to angiotensin-1. Angiotensin-1 is subsequently converted to angiotensin-2 by the enzyme angiotensin converting enzyme found in the lungs. Angiotensin-2m a potent vasoactive peptide causes blood vessels to constrict, resulting in increased blood pressure. Angiotensin-2 also stimulates the secretion of the hormone aldosterone from the adrenal cortex [9].
Aldosterone causes the tubules of the kidneys to increase the reabsorption of sodium and water into the blood. This increases the volume of fluid in the body, which also increases blood pressure. If the renin-angiotensin-aldosterone system is too active, blood pressure will be too high. Many drugs interrupt different steps in this system to lower blood pressure. These drugs are one of the main ways to control high blood pressure (hypertension), heart failure, kidney failure, and harmful effects of diabetes. It is believed that angiotensin-1 may have some minor activity, but angiotensin-2 is the major bioactive product. Angiotensin-2 has a variety of effects on the body: throughout the body, it is a potent vasoconstrictor of arterioles [9].
How the kidneys increase circulating blood volume
Angiotensin-2 also stimulates the adrenal gland to secrete a hormone called aldosterone. Aldosterone stimulates more Na reabsorption in the distal tubule, and water gets reabsorbed along with the Na. The increased Na and water reabsorption from the distal tubule reduces urine output and increases the circulating blood volume. The increased blood volume helps stretch the heart muscle and causes it to generate more pressure with each beat, thereby increasing the blood pressure. The circulating blood volume is directly proportional to the stretch of the heart muscle.
The actions taken by the kidney to regulate blood pressure are especially important during traumatic injury, when they are necessary to maintain blood pressure and conserve the loss of fluids. The body stores calcium in the bones, but also maintains a constant level of calcium in the blood. If the blood calcium level falls, then the parathyroid glands in the neck release a hormone called parathyroid hormone. Parathyroid hormone increases calcium reabsorption from the distal tubule of the nephron to restore the blood calcium level. Parathyroid hormone aside from stimulating calcium release from bone also causes calcium absorption from the intestine.
Vitamin D is also required by the body to stimulate calcium absorption from the kidney and intestine. Vitamin D is found in milk products. A precursor to vitamin D (cholecalciferol) is made in the skin and processed in the liver. The last phase in the conversion of an inactive form of cholecalciferol into active vitamin D takes place in the proximal tubule of the nephron. Once activated, vitamin D stimulates calcium absorption from the proximal tubule and from the intestine, thereby increasing blood calcium levels.
Kidney stones are abnormalities usually caused by problems in the kidney’s ability to handle calcium. In addition, the kidney’s role in maintaining blood calcium is important in the bone disease osteoporosis that afflicts many elderly people, especially women.
The kidneys therefore function in the body to:
• Control the composition of the blood and eliminate wastes by filtration/reabsorption/secretion
• Influence blood pressure by renin secretion
• Help regulate the body’s calcium by vitamin D activation
If for any reason, the kidneys fail to function, then renal dialysis methods (artificial filtration methods) becomes the only alternative to assist the patient to survive by cleansing the blood. This is especially necessary when both kidneys fail.
Mechanisms of blood pressure control by the kidneys
1. Intra-renal actions of the renin-angiotensin system in blood pressure control
The renin-angiotensin system (RAS) is a potent modulator of blood pressure, and dysregulation of the RAS results in hypertension. Pharmacological blockade of the RAS with renin inhibitors, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin receptor blockers effectively lowers blood pressure in a substantial proportion of patients with hypertension [10], reflecting the important role for RAS activation as a cause of human hypertension. While in rodents, deletion of RAS genes lowers blood pressure, overexpression causes hypertension [11].
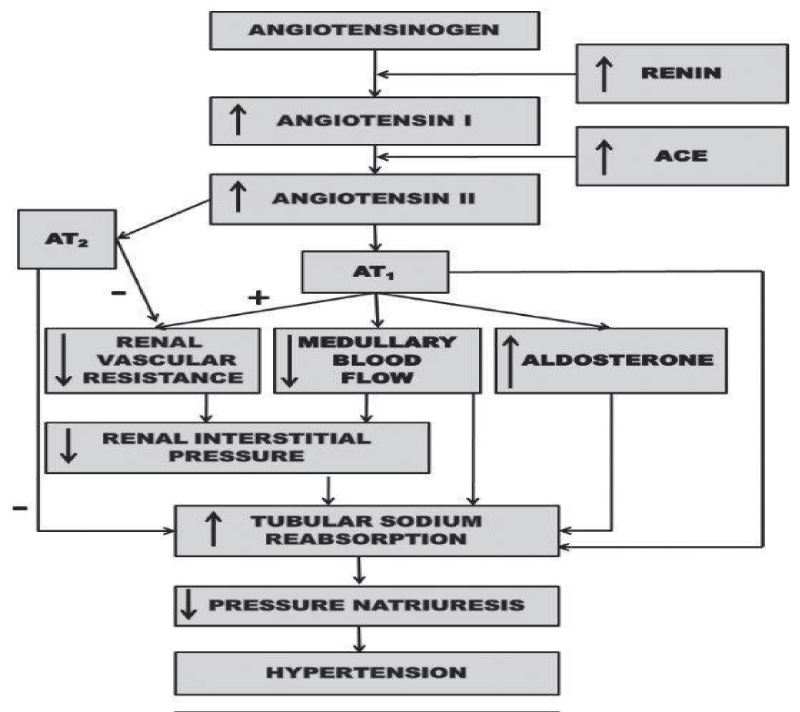
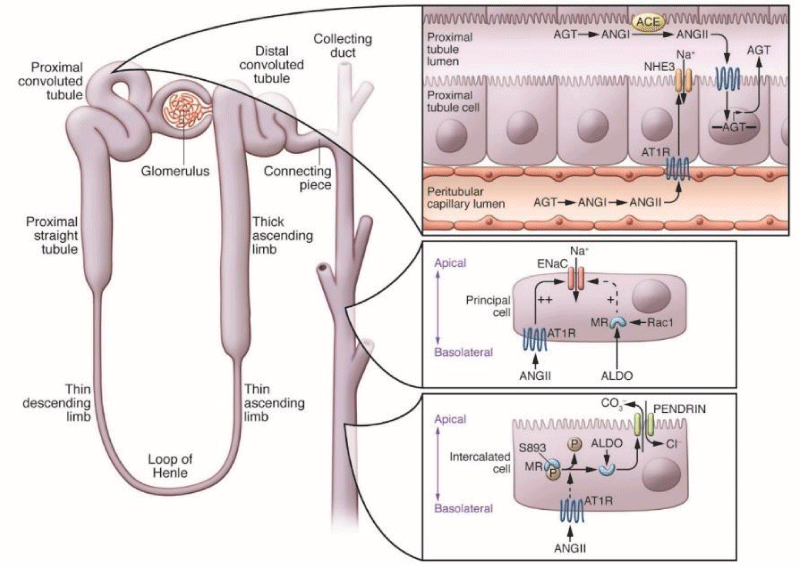
While The distal tubule cells (macula densa) sense the Na in the filtrate, and the arterial cells (juxtaglomerular cells) sense the blood pressure. Studies have shown that chronic infusion of low doses of angiotensin II directly into the kidney caused hypertension with impaired natriuresis due to a shift of the pressure-natriuresis relationship [12]. It is also believed that the existence of local and independent control of RAS activity within the kidney influencing sodium excretion and blood pressure regulation. In this hypothesis, increased circulating levels of angiotensin II are associated with accumulation of angiotensin peptides in the kidney, upregulated expression of angiotensinogen, the primary RAS substrate, in proximal tubule epithelium, and increased excretion of angiotensinogen and angiotensin peptides in urine [13]. In this feed-forward pathway, angiotensin II acting via type 1 angiotensin (AT1) receptors in the kidney induces local activation of the RAS inside the kidney and increases generation of angiotensin II in the lumen of renal tubules, resulting in autocrine and paracrine stimulation of epithelial transporters [14,15].
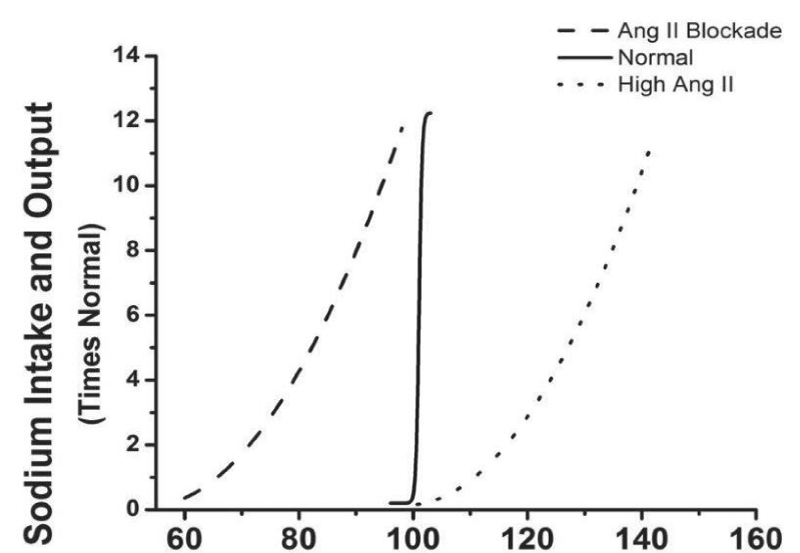
Recent studies in support of this idea have verified the critical requirement of ACE within the kidney to fully manifest stimulation of sodium transporter expression, renal sodium reabsorption, and hypertension in the setting of RAS activation [16,17] (Figures 1,2).
Figure 1: Renal mechanism whereby activation of the renin-angiotensin system reduces pressure natriuresis relationship and leads to hypertension [39].
Figure 2: A model for local control of RAS activity within the kidney- High levels of angiotensin II (ANGII) in circulation, derived from angiotensinogen (AGT) generated primarily by the liver, are associated with; increased ANGII in the kidney, up regulation of AGT in the proximal tubule epithelium, increased levels of AGT in the tubular lumen, generation of ANGII requiring angiotensin-converting enzyme (ACE) expression in the brush border of the proximal tubule (PT), and increased excretion of AGT and ANG peptides in urine [39].
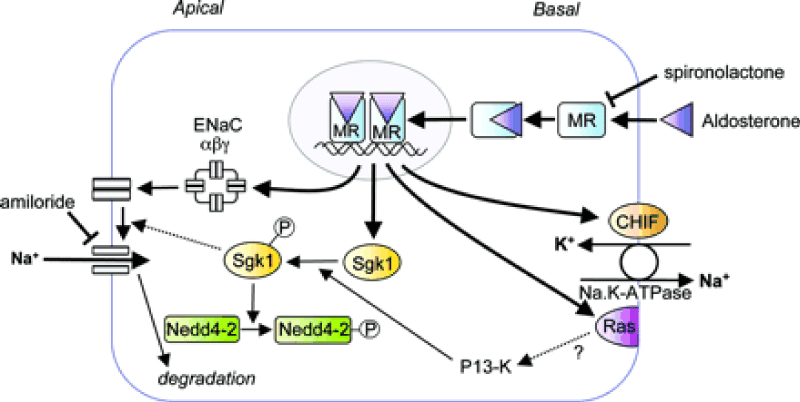
2. Novel Control Mechanisms and Sites of Action for Aldosterone in Hypertension
AT1 receptors in the zona glomerulosa of the adrenal gland stimulate aldosterone release, making aldosterone a downstream effector of the RAS. Activation of the mineralocorticoid receptor (MR) in aldosterone-sensitive nephron segments stimulates assembly and translocation of the subunits of the ENaC. Mutations in ENaC subunits that impair its degradation result in enhanced membrane density and open probability of the channels, resulting in Liddle’s syndrome, characterized by severe, early onset hypertension resembling hyper-aldosteronism, but with low levels of aldosterone [18]. Similarly, activating mutations in the gene encoding the MR also cause hypertension that is exacerbated by steroid hormone alterations during pregnancy [19]. These syndromes may highlight the capacity for dysregulation of the MR/ENaC signaling pathway in the kidney to promote hypertension.
Aldosterone, in addition to stimulation of sodium reabsorption, promotes secretion of potassium into urine. Shibata et al have shown in their studies that regulated phosphorylation of the MR modulates aldosterone responses in the kidney. They showed that phosphorylation of S843 on the MR prevents ligand binding. This form of the MR is present only in intercalated cells of the collecting duct of the kidney where its phosphorylation is differentially regulated by volume depletion and hyperkalemia. For example, in volume depletion, the MR in intercalated cells is dephosphorylated, resulting in potentiation of chloride and sodium reabsorption, allowing a distinct response to volume depletion [20]. Although the MR is classically activated by aldosterone, recent studies suggest that the small GTPase Rac1 may promote hypertension through an MR-dependent pathway, even in the setting of suppressed aldosterone levels (Figure 3).
Figure 3: Representation of an aldosterone-responsive epithelial cell. The proteins encoded by aldosterone-induced genes are discussed in the text: ENAC α, β, and γ, CHIF, sgk, and RAS are indicated are their known or putative functions [39].
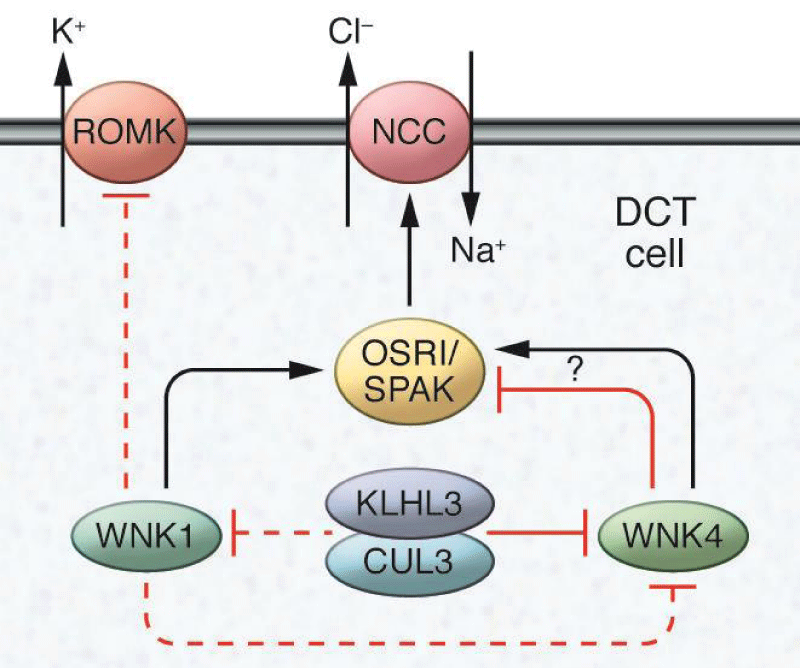
3. The WNKs: Novel Pathways Regulating Renal Solute Transport
Reliable evidence implicating a predominant role for the kidney in the regulation of blood pressure have defined the genetic basis of virtually all of the known Mendelian disorders associated with abnormal blood pressure phenotypes in humans [20-22]. In each case, these mutations impact sodium and fluid reabsorption along the nephron [21]. One of these disorders is pseudo-hypo-aldosteronism type II (PHAII), a Mendelian syndrome characterized by the unusual combination of hypertension and hyperkalemia, found to be caused by mutations in the genes encoding WNK1 (with no lysine [K]) kinase and WNK4 [22]. This discovery triggered intense study of these unique kinases, identifying roles for WNK1 and WNK4 in the regulation of sodium and potassium flux in the distal nephron. These actions are primarily mediated through control of the relative levels and activities of the thiazide-sensitive Sodium (Na) Chloride Cotransporter (NCC) and/or the Renal Outer Medullary Potassium (K) channel (ROMK) [23,24]. The NCC represents a major pathway for sodium reabsorption in the distal nephron and is the target for thiazide diuretics, which are effective and widely used antihypertensive agents [25]. Thiazides are a mainstay of treatment for PHAII, consistent with findings that NCC over-activity is a key feature of the disorder [26]. It is worth noting that while the actions of WNK4 to suppress ROMK activity have been consistent in these studies, variable effects of WNK4 on NCC activity have been observed, perhaps relating to the relative levels of WNK4 in experimental systems. In this regard, mutations causing accumulation of endogenous WNK4 enhance NCC activity possibly through phosphorylation of STE20/SPS-1-related proline-alanine-rich protein kinase (SPAK), whereas deliberate overexpression of WNK4 appears to target NCC for lysosomal degradation [24,27,28] (Figure 4).
WNK family kinases control the activity of the sodium chloride cotransporter (NCC) and the renal outer medullary potassium channel (ROMK) in distal convoluted tubule (DCT) cells in the kidney. WNK1 phosphorylates and stimulates the SPS1-related proline/alanine-rich kinase (SPAK) and oxidative stress-responsive kinase 1 (OSR1) protein kinases, which in turn, promotes NCC-dependent sodium transport. WNK1 may also inhibit ROMK. WNK4 inhibits ROMK but has been reported to have both stimulating and inhibitory actions on NCC depending on the experimental system used. Levels of WNK4 are regulated by the activity of the cullin 3-KLHL3 ubiquitin ligase, which has also been suggested to modulate WNK1.
4. How sodium and potassium flux in the distal nephron is regulated.
Enhanced activity of NCC through modulation of WNKs seems to be a final common pathway for the development of hypertension in a number of scenarios. For example, β-adrenergic stimulation increases blood pressure by suppressing WNK4 and, in turn, enhancing NCC activity [29]. In addition, calcineurin inhibitors commonly used to treat autoimmune disease and prevent transplant rejection, frequently cause hypertension. Recent studies by Ellison et al indicate that the mechanism of hypertension associated with calcineurin inhibitor use involves stimulation of NCC through upregulation of WNK3 [30].
While the ongoing delineation of WNK functions has provided significant insights into kidney physiology, only a small subset of patients with PHAII have mutations in WNK genes. Using exome sequencing, Lifton’s group uncovered mutations in the kelch-like 3 (KLHL3) and cullin 3 (CUL3) genes in patients with PHAII [31]. Moreover, mutations in these two genes accounted for disease in approximately 80% of individuals affected with PHAII [31]. KLHL3 is one of a family of more than 50 broad-complex, tramtrack, bric-a-brac complex–containing (BTB-containing) kelch proteins, characterized by six-bladed, β-propeller domains for binding specific target proteins. CUL3 provides the scaffold for the complex, which includes BTB-domain proteins such as KLHL3 and a RING domain protein that serves as an E3 ubiquitin ligase, targeting specific protein substrates for ubiquitination [32] (Figure 5).
Figure 5: Effect of changes in mean arterial pressure during chronic changes in sodium intake after angiotensin-converting enzyme (ACE) inhibition, or when angiotensin II was infused at a constant low dose (5 ng/ kg/min) to prevent angiotensin II from being suppressed when sodium intake was raised. (Redrawn from data in Hall et al, 1980) [33].
5. Salt Homeostasis
Salt sensitivity, defined as an exaggerated change in blood pressure in response to extremes in dietary salt intake, is relatively common and is associated with an increased risk for the development of hypertension. Classic Guytonian models suggest that a defect in sodium excretion by the kidney is the basis for salt sensitivity, with impaired elimination of sodium during high-salt feeding leading directly to expanded extracellular fluid volume, which promotes increased blood pressure [34]. This model presumes that the two major components of extracellular volume within the intravascular and interstitial spaces are in equilibrium. As such, accumulation of sodium would be accompanied by commensurate retention of water to maintain iso-osmolality and would thereby proportionally expand the intravascular volume.
However, studies by Titze et al. recently indicated that sodium handling is more complex than this classical two-compartment model; the interstitium of the skin may act as a sodium reservoir, buffering the impact of sodium accumulation on intravascular volume and blood pressure [35]. During high-salt feeding, sodium accumulates in the subdermal interstitium at hypertonic concentrations in complexes with proteoglycans [35,36]. Macrophages infiltrating the interstitial space sense hypertonicity caused by this accumulation of sodium in excess of water, triggering expression of TonEBP, a transcription factor regulating the expression of osmo-protective genes. One of the genes induced downstream of TonEBP is vascular endothelial growth factor-C (VEGF-C) [35], a potent inducer of lymph angiogenesis.
In response to high-salt feeding, Titze’s group found robust lymphatic vessel hyperplasia in the dermal interstitium [35]. Depletion of macrophages, cell-specific deletion of TonEBP from macrophages, or specific blockade of VEGF-C prevented hyperplasia of lymphatic vessels and enhanced the level of sodium-dependent hypertension [35-37] demonstrating that this pathway has a key role in the extrarenal control of sodium and fluid volumes. Elevated plasma level of VEGF-C in patients with refractory hypertension was observed, indicating that this system might be perturbed in the human disorder. However, pre-clinical models predict that reduced levels of VEGF-C would promote hypertension [38]. Nonetheless, chronic hypertension in humans is a complex disorder; it is possible that the observed elevation in VEGF-C levels may reflect tissue resistance to VEGF-C or even a compensatory response.
Hypertensive kidney injury and the progression of chronic kidney disease
The kidney remains a major site for hypertensive target organ damage which is second only to diabetic nephropathy as a primary cause for end-stage renal disease (ESRD). Moreover, the presence of chronic kidney disease (CKD), including that caused by hypertension, has been shown to be a strong independent risk factor for adverse cardiovascular outcomes. Nevertheless, major aspects of clinical hypertensive renal disease remain poorly understood such as the marked differences in individual susceptibility to hypertensive renal damage and the apparent variable reno-protective effectiveness of antihypertensive classes [40].
Studies have revealed that time-varying SBP was associated with incident CKD, with a steady increase in risk of incident CKD above an SBP of 120 mmHg. Time-weighted SBP was associated with a more rapid decline of kidney function. Diabetes was the strongest predictor of incident CKD, and more rapid decline of kidney function and worse glycemic control were associated with greater risk, thereby supporting the role of BP and other traditional risk factors like diabetes in the initiation and progression of kidney function decline in hypertensive patients with normal kidney function at baseline [41].
Discussion
Sodium handling by the kidney is a major determinant of the level of intra- and extra- renal blood pressure, and its under complex physiological control by hormones, inflammatory mediators, and the sympathetic nervous system. It is self-evident that a basic mechanism of efficacy for diuretics and dietary sodium restriction in hypertension is to favorably influence sodium balance and homeostasis. Other antihypertensive agents such as RAS inhibitors, vasodilators, and β-blockers work through a similar mechanism by facilitating pressure-natriuresis. Recent studies have also suggested that WNK signaling pathways, soluble inflammatory mediators, and pathways regulating extra-renal sodium disposition might also be useful targets for enhancing elimination of sodium and reducing blood pressure in hypertension.
The renin-angiotensin system (RAS) is a powerful modulator of blood pressure, and dysregulation of the RAS causes hypertension. Pharmacological blockade of the RAS with renin inhibitors, angiotensin-converting enzyme (ACE) inhibitors, or angiotensin receptor blockers effectively lowers blood pressure in a substantial proportion of patients with hypertension [10], reflecting the important role for RAS activation as a cause of human hypertension. Similarly, in rodent models, deletion of RAS genes lowers blood pressure whereas overexpression causes hypertension [11].
Conclusion
There is essential link between the kidney and blood pressure control. An impaired capacity of the kidney to excrete sodium in response to elevated blood pressure is a major contributor to hypertension, irrespective of the initiating cause. In this regard, novel pathways controlling key sodium transporters in kidney epithelia have a critical impact on hypertension pathogenesis, supporting a model in which impaired renal sodium excretion is a final common pathway through which vascular, neural, and inflammatory responses raise blood pressure. The relationship between sodium intake and changes in body fluid volume reveals the mechanism.
Recommendation
Expanded understanding of the role of the kidney as both a cause and target of hypertension to increase knowledge on key aspects of pathophysiology may help lead to identification of new strategies of regulating both intra-and extra- renal blood pressure to help in the prevention and treatment of hypertension.
References
- Osborn JW, Fink GD, Kuroki MT. Neural mechanisms of angiotensin II-salt hypertension: implications for therapies targeting neural control of the splanchnic circulation. Curr Hypertens Rep. 2011; 13: 221-228. Ref.: https://tinyurl.com/y8axh8v9
- Guyton AC. Blood pressure control -- special role of the kidneys and body fluids. Science. 1991; 252: 1813-1816. Ref.: https://tinyurl.com/y8fxexxe
- McCurley A. Direct regulation of blood pressure by smooth muscle cell mineralocorticoid receptors. Nat Med. 2012; 18: 1429-1433. Ref.: https://tinyurl.com/ybqzj4mf
- Dahl LK, Heine M, Thompson K. Genetic influence of the kidneys on blood pressure. Evidence from chronic renal homografts in rats with opposite predispositions to hypertension. Circ Res. 1974; 40: 94-101. Ref.: https://tinyurl.com/ycvplgse
- Matsusaka T, Niimura F, Shimizu A, Pastan I, Saito A, et al. Liver angiotensinogen is the primary source of renal angiotensin II. J Am Soc Nephrol. 2012; 23: 1181-1189. Ref.: https://tinyurl.com/y7g4q6vp
- Lawes C M, Vander Hoorn S, Rodgers A, International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet. 2008; 371: 1513-1518. Ref.: https://tinyurl.com/ycahczth
- Wolf-Maier K, Cooper RS, Banegas JR, Giampaoli S, Hense HW, et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA. 2003; 289: 2363-2369. Ref.: https://tinyurl.com/yc2wugnx
- Gu Q, Burt V L, Dillon C F, Yoon S. Trends in antihypertensive medication use and blood pressure control among United States adults with hypertension: The National Health And Nutrition Examination Survey, 2001 to 2010. Circulation. 2012; 126: 2105-2114. Ref.: https://tinyurl.com/yb6cmatp
- Hani MW, Stephen CT. The role of the kidney in regulating arterial blood pressure. Nat Rev Nephrol. 2012; 8: 602-609. Ref.: https://tinyurl.com/y9jfdefu
- Matchar DB, McCrory DC, Orlando LA, Patel MR, Patel UD, et al. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers for treating essential hypertension. Ann Intern Med. 2008; 148: 16-29. Ref.: https://tinyurl.com/y7zxfcr4
- Le TH, Coffman TM. Targeting genes in the renin-angiotensin system. Curr Opin Nephrol Hypertens. 2008; 17: 57-63. Ref.: https://tinyurl.com/ycprl2fd
- Hall JE. Control of sodium excretion by angiotensin II: intrarenal mechanisms and blood pressure regulation. Am J Physiol. 1986; 250: R960-R972. Ref.: https://tinyurl.com/y8rhrkfy
- Kobori H, Nangaku M, Navar LG, Nishiyama A. The intrarenal renin-angiotensin system: from physiology to the pathobiology of hypertension and kidney disease. Pharmacol Rev. 2007; 59: 251-287. Ref.: https://tinyurl.com/yd4qe48e
- Navar LG, Lewis L, Hymel A, Braam B, Mitchell KD. Tubular fluid concentrations and kidney contents of angiotensins I and II in anesthetized rats. J Am Soc Nephrol. 1994; 5: 1153-1158. Ref.: https://tinyurl.com/y8zz6bac
- Navar LG, Harrison-Bernard LM, Wang CT, Cervenka L, Mitchell KD. Concentrations and actions of intraluminal angiotensin II. J Am Soc Nephrol. 1999; 10: S189-S195. Ref.: https://tinyurl.com/ydy6nvlk
- Gonzalez-Villalobos RA, Billet S, Kim C, Satou R, Fuchs S, et al. Intrarenal angiotensin-converting enzyme induces hypertension in response to angiotensin I infusion. J Am Soc Nephrol. 2011; 22: 449-459. Ref.: https://tinyurl.com/y9wvwdm8
- Gonzalez-Villalobos RA, Janjoulia T, Fletcher NK, Giani JF, Nguyen MT, et al. The absence of intrarenal ACE protects against hypertension. J Clin Invest. 2013; 123: 2011-2023. Ref.: https://tinyurl.com/y9u87rcm
- Tamura H, Schild L, Enomoto N, Matsui N, Marumo F, et al. Liddle disease caused by a missense mutation of beta subunit of the epithelial sodium channel gene. J Clin Invest. 1996; 97: 1780-1784. Ref.: https://tinyurl.com/y862nz5l
- Geller DS, Farhi A, Pinkerton N, Fradley M, Moritz M, et al. Activating mineralocorticoid receptor mutation in hypertension exacerbated by pregnancy. Science. 2000; 289: 119-123. Ref.: https://tinyurl.com/ybklpr83
- Shibata S, Zhang J, Puthumana J, Stone KL, Lifton RP. Kelch-like 3 and Cullin 3 regulate electrolyte homeostasis via ubiquitination and degradation of WNK4. Proc Natl Acad Sci U S A. 2013; 110: 7838-7843. Ref.: https://tinyurl.com/yc2edjda
- Lifton RP, Gharavi AG, Geller DS. Molecular mechanisms of human hypertension. Cell. 2001; 104: 545-556. Ref.: https://tinyurl.com/ycg9hn6w
- Wilson FH, Disse-Nicodème S, Choate KA, Ishikawa K, Nelson-Williams C, et al. Human hypertension caused by mutations in WNK kinases. Science. 2001; 293: 1107-1112. Ref.: https://tinyurl.com/ydf9y4sd
- Kahle KT, Ring AM, Lifton RP. Molecular physiology of the WNK kinases. Annu Rev Physiol. 2008; 70: 329-355. Ref.: https://tinyurl.com/yaqqkxyw
- McCormick JA, Ellison DH. The WNKs: atypical protein kinases with pleiotropic actions. Physiol Rev. 2011; 911:177-219. Ref.: https://tinyurl.com/ycvbm4ap
- JAMA. ALLHAT Officers Coordinators for the ALLHAT Collaborative Research Group the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA. 2002; 288: 2981-2997.
- Lalioti MD, Zhang J, Volkman HM, Kahle KT, Hoffmann KE, et al. Wnk4 controls blood pressure and potassium homeostasis via regulation of mass and activity of the distal convoluted tubule. Nat Genet. 2006; 38: 1124-1132. Ref.: https://tinyurl.com/y9j66zwp
- Ahlstrom R, Yu AS. Characterization of the kinase activity of a WNK4 protein complex. Am J Physiol Renal Physiol. 2009; 297: F685-F692. Ref.: https://tinyurl.com/y7wp9frw
- Cai H, Cebotaru V, Wang YH, Zhang XM, Cebotaru L, et al. WNK4 kinase regulates surface expression of the human sodium chloride cotransporter in mammalian cells. Kidney Int. 2006; 69: 2162-2170. Ref.: https://tinyurl.com/ybhd526t
- Mu S, Shimosawa T, Ogura S, Wang H, Uetake Y, et al. Epigenetic modulation of the renal beta-adrenergic-WNK4 pathway in salt-sensitive hypertension. Nat Med. 2011; 17: 573-580. Ref.: https://tinyurl.com/ycz7lqzd
- Hoorn EJ, Walsh SB, McCormick JA, Fürstenberg A, Yang CL, et al. The calcineurin inhibitor tacrolimus activates the renal sodium chloride cotransporter to cause hypertension. Nat Med. 2011; 17: 1304-1309. Ref.: https://tinyurl.com/y9sayeqr
- Boyden LM, Choi M, Choate KA, Nelson-Williams CJ, Farhi A, et al. Mutations in kelch-like 3 and cullin 3 cause hypertension and electrolyte abnormalities. Nature. 2012; 482: 98-102. Ref.: https://tinyurl.com/y9e4opta
- Prag S, Adams JC. Molecular phylogeny of the kelch-repeat superfamily reveals an expansion of BTB/kelch proteins in animals. BMC Bioinformatics. 2003; 4: 42. Ref.: https://tinyurl.com/yakupc8a
- Hall JE, Guyton AC, Smith MJ Jr, Coleman TG. Blood pressure and renal function during chronic changes in sodium intake: Role of angiotensin. Am J Physiol. 1980; 239: F271-F280. Ref.: https://tinyurl.com/y7rglkbd
- Murphy TJ, Alexander RW, Griendling KK, Runge MS, Bernstein KE. Isolation of a cDNA encoding the vascular type-1 angiotensin II receptor. Nature. 1991; 351: 233-236. Ref.: https://tinyurl.com/y9o4xx77
- Machnik A, Neuhofer W, Jantsch J, Dahlmann A, Tammela T, et al. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C-dependent buffering mechanism. Nat Med. 2009; 15: 545-552. Ref.: https://tinyurl.com/yaabdbdf
- Machnik A, Dahlmann A, Kopp C, Goss J, Wagner H, et al. Mononuclear phagocyte system depletion blocks interstitial tonicity-responsive enhancer binding protein/vascular endothelial growth factor C expression and induces salt-sensitive hypertension in rats. Hypertension. 2010; 55: 755-761. Ref.: https://tinyurl.com/ya4qcfa6
- Wiig H, Schröder A, Neuhofer W, Jantsch J, Kopp C, et al. Immune cells control skin lymphatic electrolyte homeostasis and blood pressure. J Clin Invest. 2013; 123: 2803-2815. Ref.: https://tinyurl.com/yda6rgqh
- Yang GH, Zhou X, Ji WJ, Zeng S, Dong Y, et al. Overexpression of VEGF-C attenuates chronic high salt intake-induced left ventricular maladaptive remodeling in spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol. 2014; 306: H598-H609. Ref.: https://tinyurl.com/yc8z2nnt
- Granger JP, George EM. Role of the Kidney in Hypertension. 2012; 1086-1108. Ref.: https://tinyurl.com/y9ruk4af
- Griffin KA. Hypertensive Kidney Injury and the Progression of Chronic Kidney Disease. Hypertension. 2017; 70: 687-694. Ref.: https://tinyurl.com/yayeuxhb
- Rebecca Hanratty, Michel Chonchol, Edward Havranek P, David Powers J, Miriam Dickinson L, et al. Relationship between Blood Pressure and Incident Chronic Kidney Disease in Hypertensive Patients. Clin J Am Soc Nephrol. 2011; 6: 2605-2611. Ref.: https://tinyurl.com/y88whgoa