Review Article
Strategic Plans for Diagnosis, Treatment & Control of Hypertension

M Mohsen Ibrahim*
President of the Egyptian Hypertension Society, Professor of Cardiology, Cairo University, Egypt
*Address for Correspondence: M Mohsen Ibrahim, MD, President of the Egyptian Hypertension Society, Professor of Cardiology, Cairo University, Egypt, Tel: 00201222273816; Email: [email protected]; [email protected]
Dates: Submitted: 12 November 2018; Approved: 21 November 2018; Published: 23 November 2018
How to cite this article: Ibrahim MM. Strategic Plans for Diagnosis, Treatment & Control of Hypertension. Ann Clin Hypertens. 2018; 2: 067-078. DOI: 10.29328/journal.ach.1001013
Copyright License: © 2018 Ibrahim MM. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Two major challenges face the practicing physicians and medical community regarding the management of hypertension. First is accurate diagnosis and finding who is the truly hypertensive patient in need of life-long treatment. Second is to improve blood pressure control through addressing hypertension risk factors, adherence to treatment and frequent monitoring.
- Current Challenges in Management
o Accurate diagnosis of hypertension
o Improving blood pressure control
- What Do We Need For The Future?
Accurate Diagnosis of Hypertension
Uncomplicated essential hypertension being a silent disease without symptoms, its diagnosis depends on accurate measurement of blood pressure and obtaining readings beyond a specific threshold defines the diagnosis of hypertension. Three problems face blood pressure readings. First the accuracy of blood pressure measuring method, second blood pressure variability, third definition of hypertension diagnostic threshold. At present, there are four methods for checking blood pressure. The most popular is the clinic or office measurement using mercury sphygmomanometer or electronic oscillometric devices. This method has a number of limitations particularly with the mercury auscultatory technique because of inaccuracy of readings if adequate precautions are not taken before and during the procedure. Furthermore, office readings are influenced by the white coat effect, will miss masked hypertension and are liable to visit to visit variability. More importantly, office readings do not correlate well with target organ damage (TOD) and future cardiovascular events. Recording blood pressure over the 24 hrs- ambulatory blood pressure monitoring (ABPM) is recommended by many as the golden standard for the diagnosis of hypertension. Measurements are taken every half an hour over day (awakening) and night (sleep), identifying nocturnal dipping, and they correlated well with TOD and future cardiovascular events and can diagnose white coat and masked hypertension.
Home blood pressure measurement is the third method to diagnose hypertension. Blood pressure is checked by the patient or his relatives who are trained on the proper technique and following the necessary precautions with a calibrated and valid device. Blood pressure should be checked twice morning and evening for one week and the average of the last six days is taken.
Recent guidelines recommends out-of-office blood pressure measurements using ABPM or home blood pressure monitoring to confirm the diagnosis of hypertension [1-3]. Knowing the blood pressure of an individual outside the clinic setting is more predictive of outcomes than their clinic blood pressure [4].
The fourth method for checking blood pressure which is gaining popularity, recommended by new guidelines and used in recent clinical trials is the automated office blood pressure measurement (AOPB). Now, there is evidence to consider replacing manual office blood pressure with AOBP [4]. For AOBP, multiple readings are taken at one minute interval with a fully automated electronic oscillometric device while the patient is resting quietly alone without interruption in a separate room. The awaken (daytime) ABPM correlates significantly with AOBP [5]. Automated devices produce readings that differ from readings with manual technique. Many patients would have been misclassified as having hypertension using routine manual office blood pressure compared with AOBP [5]. WHO recommended the use of a validated semi-automated oscillometric device for clinics in low resource settings because of the inherent inaccuracy of the auscultatory technique [6]. The World Hypertension League (WHL- 2014) [7] recommends, in community screening, a semi-automated or fully automated oscillometric blood pressure device. There is a significant correlation between LV mass index, intimal media thickness of carotid artery and AOBP but not with manual blood pressure [8].
AOBP measurement avoids auscultation induced errors and minimizes white-coat hypertension effects, as measures can be taken without a doctor or a nurse present. AOBP measurement has been shown to have a good correlation with home and daytime ABPM. Recently it has been shown that the patient does not have to be alone to obtain an accurate reading.
All automated devices require regular maintenance to ensure accurate reading. The WHL has developed a policy statement to support using automated devices for assessment of blood pressure [7].
Definition of hypertension
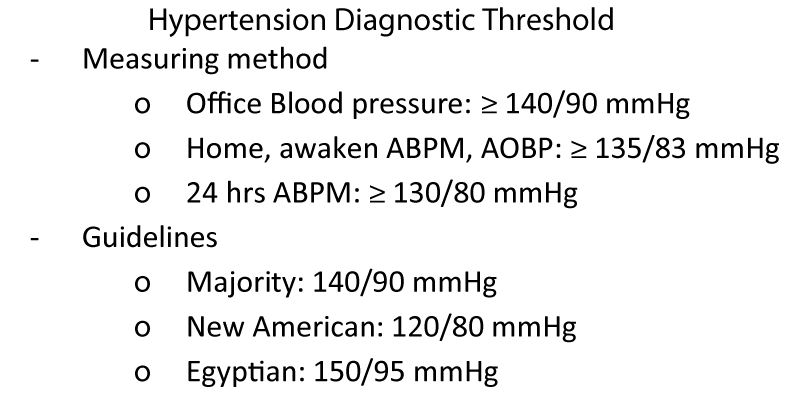
The cut off point for diagnosing hypertension differs according to the method of measurement and between different guidelines. Average office blood pressure readings should be taken after 5- minute rest and following the recommendations for accurate reading. Measurements are to be repeated more than twice and taken on two or more office visits with a calibrated device and proper cuff size. Blood pressure levels ≥ 140/90 mmHg defines the diagnosis of office hypertension in most of the guidelines. The cut off for awakened (day time) ABPM, average home reading and AOBP is 135/85 mmHg, while for 24 hrs ABPM, the diagnostic cut off for hypertension is 130/80 mmHg. Whereas the diagnostic threshold for office readings has been set at 140/90 mmHg for most guidelines, the new American guidelines [9] set a level 120/80 mmHg as the limit of normal blood pressure. Levels exceeding 120/80 mmHg were considered abnormal and stage 1 hypertension if SBP is 130-139 mmHg or DBP 80-89 mmHg and stage II if ≥ 140/90 mmHg.
These cut off points seem unrealistic for many countries and will classify millions of individuals as being hypertensive. The American guidelines were possibly influenced by the results of the SPRINT trial [10] which showed that aggressive lowering of blood pressure to target less than 120/80 mmHg is associated with a better cardiovascular outcome and decreased mortality compared with the standard 140/90 mmHg. SPRINT results apply to a specific patients population- older than 50 years, SBP ≥ 130/80 mmHg with no diabetes and at high cardiovascular risk. The technique of measuring blood pressure in SPRINT was not the standard office technique. Extrapolation to office practices of SPRINT results is difficult. Advocating a target of 120 mmHg is not justified in clinical practice, increasing the costs of increasing clinic visits and more medications (Figure 1).
Although most of the guidelines recommend a SBP of 140 mmHg as the usual hypertension threshold, this in many parts of the world could put an excessive burden on limited budgets.
Rationale for a diagnostic threshold of 150/95 mmhg [11-17]
• The diagnostic threshold of 140/90 mmHg is neither evidence-based nor universally accepted.
• At the 17th World Conference of Hypertension League Council (1997), 13 out of 27 national hypertension societies stayed with 160/95 mmHg.
• The distress about having hypertension and possibly requiring life-long drug therapy may lead to development of anxiety symptoms.
• The threshold of 140/90 mmHg was based upon data from research studies and drug trials where blood pressure readings were taken for research purposes and do not actually routine office measurements.
• Data derived from several large studies have equated a manual (research quality) office blood pressure of 140/90 mmHg with a mean awake ambulatory blood pressure (ABP) of 135/85 mmHg. There was a consistent difference between the mean awake ABP and the routine office blood pressure greater than the usual recognized 5 mmHg (140/90 mmHg for office blood pressure vs. 135/85 mmHg for mean awake ABP). Blood pressure measurement in routine clinical practice seems to be at least 10/5 mmHg higher than the research-quality office blood pressure.
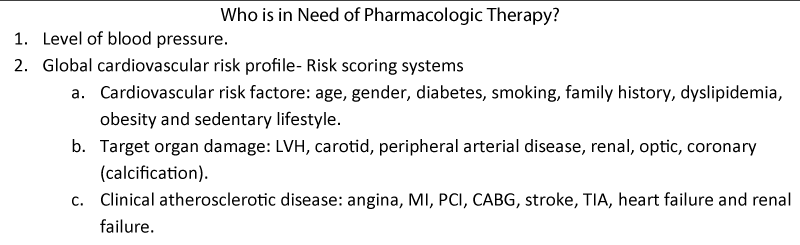
Who is in need of pharmacologic therapy?
The decision to initiate pharmacologic therapy in a hypertension patient should not be taken lightly. Since once initiated drug therapy will continue for the rest of patient life. Level of blood pressure is only one factor in the decision making. The particular SBP that signals the need for treatment initiation and SBP treatment goals remains uncertain. Decision to initiate drug therapy should consider in addition to blood pressure level, the global cardiovascular risk profile of the patient. This risk profile is determined by the presence of target organ damage, symptomatic atherosclerotic cardiovascular disease (coronary, cerebral, peripheral) and other cardiovascular risk factors such as age, gender, family history, diabetes, dyslipidemia, cigarette smoking, obesity, CKD, sedentary lifestyle and continued work and family stresses. WHO [18] suggests performing cardiovascular risk stratification according to WHO/ISH risk prediction charts using a limited pannel of data (age, gender, SBP, type 2 diabetes, smoking and total serum cholesterol).
In individuals at low cardiovascular risk (no cardiovascular risk factors or TOD) with blood pressure 140-160 mmHg, lifestyle modification and regular blood pressure monitoring may be enough. Levels of SBP ≥ 160 mmHg even in low risk patients will need lifelong therapy, if they persist on repeated measurements. A major issue is to choose cardiovascular disease risk thresholds that can maximize events prevented without increasing the total numbers treated in a defined population. However, there is a problem when assessing cardiovascular risk in populations for which cohort data are not available and calculation of cardiovascular risk along current western-based risk factors cannot be calibrated.
Pharmacotherapy for mild hypertension
Cochrane Review [19] (Figure 2)
• The effects of antihypertensive drug therapy on mortality and morbidity in adults with mild hypertension (systolic blood pressure 140-159 mmHg and/or diastolic blood pressure 90-99 mmHg and without cardiovascular disease was examined.
• The Cochrane review (2012) used individual patient meta-analysis to identify all patients with mild hypertension studied in randomized trials and suitable for primary prevention.
• This review found that compared with a placebo, treatment with an antihypertensive drug did not reduce any outcome, including total mortality, total cardiovascular events, coronary heart disease or stroke.
• Based on the best available evidence at the present time, this review does not show any significant benefit of antihypertensive drug therapy in reducing mortality, heart attacks, strokes or overall cardiovascular event in this group.
• Treatment caused 9% of patients to discontinue treatment due to adverse effects.
• It therefore remains uncertain whether treatment is beneficial, neutral or harmful for the population.
• More RCTs are needed in this prevalent population to know whether the benefits of treatment exceed the harms.
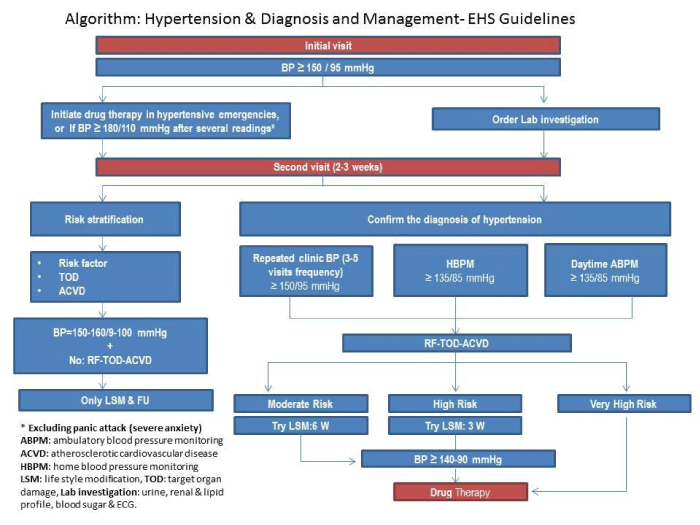
Because individual blood pressure measurements tend to vary in an unpredictable or random fashion, a single reading is inadequate for clinical decision- making. An average of 2 to 3 blood pressure measurements obtained on 2 to 3 separate occasions will minimize random error and provide more accurate basis for estimation of blood pressure [9]. The number of blood pressure measurements can influence the classification of patients as hypertensive. Additional research is needed to better define blood pressure treatment goals, especially in specific populations, including age, sex, race, ethnicity and comorbid conditions. The approach of Canadian guidelines is to allow patients without TOD or increased cardiovascular risk to be diagnosed at the third office visit if clinic blood pressure remained ≥ 160/100 mmHg because the greatest decrease in blood pressure was shown to occur between visit 1 and 2. If the blood pressure at visit 3 was 140-159/90-99 mmHg, up to 3 additional visit over 6 months period is required to diagnose a patient as hypertensive. See algorithm of the EHS at the end of statement.
Improving blood pressure control
Less than half of individuals who are aware of having a diagnosis of elevated blood pressure receive treatment. Among those who receive treatment only one third have their blood pressure controlled. Prevalence of uncontrolled hypertension is high and increasing in many developing countries. Up to 50% of patients quit the treatment within the first year [20], in Egypt discontinuation rate exceeds 70% [21]. In some studies only 10 to 15% of originally treated patients were still adherent to drug therapy after 5 or more years [22].
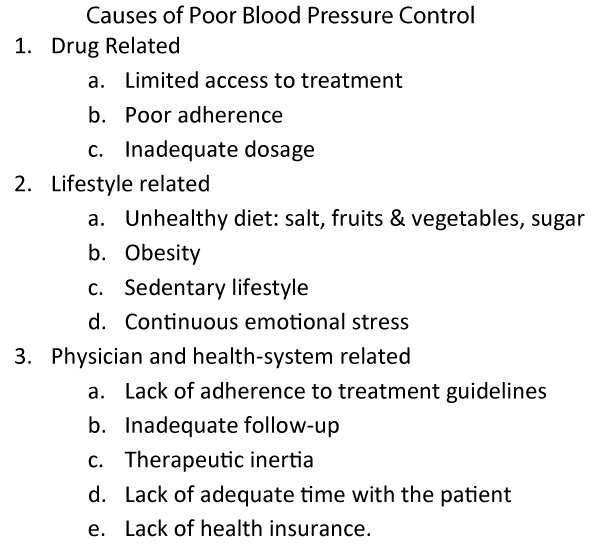
Causes of poor blood pressure control are drug, lifestyle, physician and health-system related. Drug related causes are limited access to treatment, poor adherence to medication, inadequate dosages and improper combinations. Reasons of poor adherence to pharmacologic therapy include long duration of therapy, the silent symptoms-less nature of hypertension, side effects of medications, complicated drug regimens, too many tablets, frequent dosing, drug cost, lack of motivation, forgetfulness, personal disapproval of medicines, fear of potential harm, other priorities, poor understanding of the condition, absence of follow-up and feeling of no immediate benefit. Doctors' inertia and failure to prescribe adequate drug dosage, to increase dosage or add additional drug can also lead to poor blood pressure control.
On the other hand, poor blood pressure control can be due to unhealthy lifestyle e.g. failure to control obesity, exercise or to follow a healthy diet with limited salt intake (< 2 gm sodium/ day) and adequate amount (5 or more servings/ day) of fruits and vegetables, avoiding emotional stress and sedentary lifestyle. Consumptions of high sodium content foods are increasing in developing countries secondary to the popularity of fast food restaurants. WHO recommends that adults should consume less than 2 gm of sodium (5gm of salt) and at least 3.5 gm of potassium per day [23].
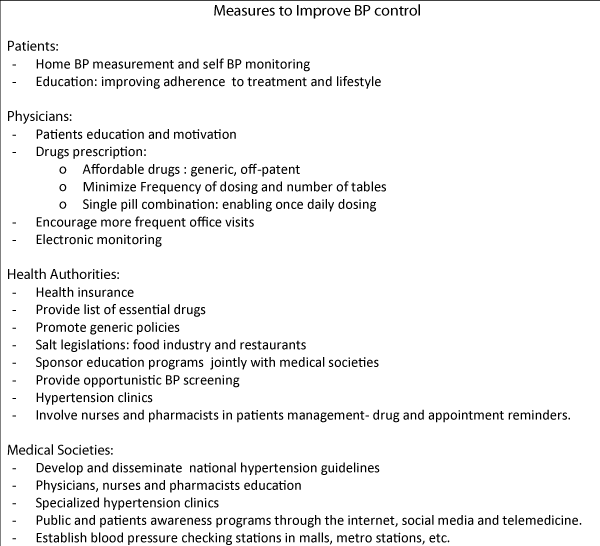
Physician and health system causes of poor control include lack of adherence to guidelines, inadequate follow-up, lack of adequate time with the patient, therapeutic inertia and lack of health insurance (Figure 3).
Measures to improve blood pressure control
Health authorities, physicians, drug industry and scientific medical societies should collaborate to improve blood pressure control. Health insurance is almost non-existent in many developing countries, patients have to purchase antihypertensive drugs out if their own pocket which is an important cause of discontinuation of therapy in poor patients. Health authorities and specialized medical societies can develop specialized hypertension clinics providing free medical services. In Egypt, the Egyptian Hypertension Society (EHS) in collaboration with industry have established a number of hypertension clinics in many universities and Ministry of Health hospitals.
Psychosocial, economic factors and health illiteracy contribute to poor drug compliance. Societies can organize group education sessions and prepare printed information material, to create patients motivation and encourage self-recording of blood pressure. Patients can be taught to measure and monitor their blood pressure with validated devices (Figure 4).
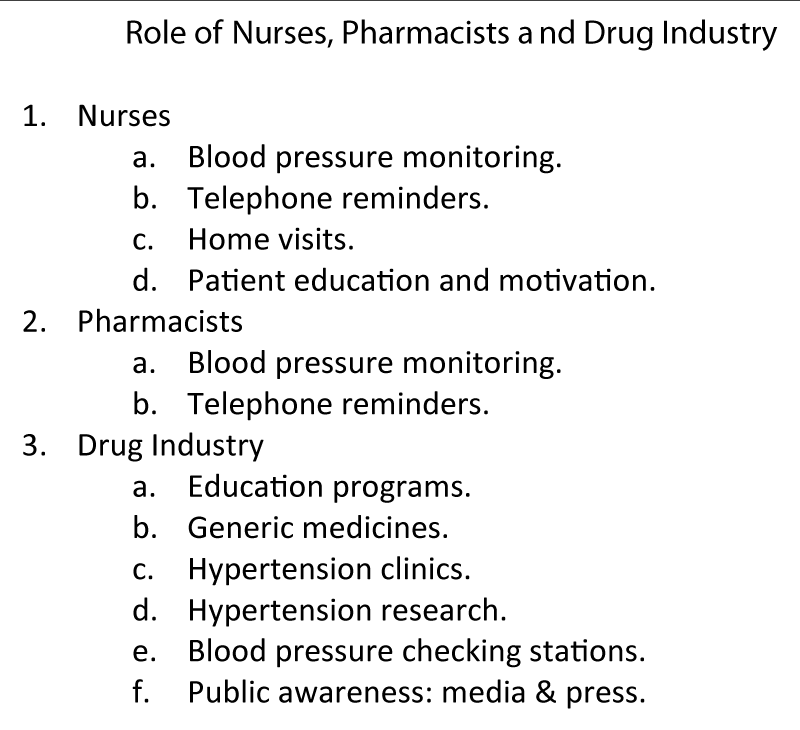
Physicians play a central role in improving adherence to treatment through patient education, simplification of dosing regimen, prescription of affordable and available drugs. Minimizing frequency of dosing and number of tablets improve patient adherence. Patient adherence is better to once-daily regimen than 2 or more doses/day. Single pill combinations enable once-daily dosing. Also, physicians can provide correct information to the patient on the risks of hypertension and benefits of the therapy and on the goals to be achieved. Educating the patient is a key component to improving adherence. Nurses can improve adherence to treatment [24], through patient education, telephone reminder of clinic appointment and medicine intakes. Paying home visits proved successful in improving control. Other approaches to improve drug adherence include: pill organizers and electronic monitoring methods for assessing drug adherence with medication through event monitoring system (MEMS) which stores times and dates of each opening of the drug package. A team-based hypertension care involving nurse or pharmacist intervention demonstrated reductions in blood pressure and/or greater achievement of blood pressure goals when compared with usual care [25]. A combination program involving self- blood pressure monitoring, reminders, educational material and a pharmacist/nurse help were the most cost effective methods of improving adherence with antihypertensive therapy. More frequent office visits specially for newly treated patients is recommended (Figure 5).
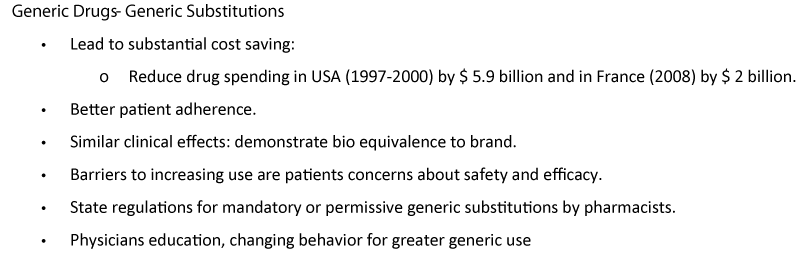
Health authorities should prepare a list of essential drugs and develop legislation to promote generic market entry. List is guide for national committees responsible for identification of the most cost- effective medicines at national level. Updating the list and promoting generic and off-patent medicines can generate large savings. In France, implementation of a general generic substitution strategy saved nearly 2 billion US dollars in 2008 [26].
National hypertension guidelines
The absence of specific national hypertension treatment guidelines based on country specific circumstances adds to the challenges in hypertension management. Medical societies should develop national guidelines for management of hypertension in poor resource settings. Implementation of the European and American guidelines will label a large number of individuals as in need of medical therapy and follow-up. This will result in over-medication, difficulties in resources allocation and failure of sustainability. Guidelines should provide cost-effective screening, diagnosis and treatment for hypertension. Evidence based guidelines does not inform the clinician to what extent a recommended cut-off point represents a valid demarcation line in relation to each population or individual. Risk of high blood pressure will depend not only on the level of blood pressure, but more importantly on the global cardiovascular risk profile. Exporting research results and intervention methods from industrialized countries ignores the fact that expectations, costs and burden of disease vary between developed and developing countries. USA spends more than $ 8362 per capita on health, whereas Eritrea spends less than $ 12 per capita [27]. Guidelines should include drug affordability as main management component and provide algorithms for detecting and managing hypertension at the community level. The development of the Egyptian Hypertension Guidelines [28], could serve as an example for developing countries (EHS Algorithms). Many developing countries with limited resources cannot treat everyone with a blood pressure beyond the defined threshold (≥ 140/90 mmHg).
Recommendations made for more prosperous nations cannot fully apply to all communities or to low and middle income countries.
The absence of treatment guidelines in most developing countries is associated with the prescription of drugs based upon Drug Company or medical representatives recommendations who may not have adequate qualifications or who have financial incentives for certain prescribing patterns.
Blood pressure monitoring
Frequent blood pressure monitoring is an essential component in management of hypertension and improving blood pressure control. Monitoring can be done by the patient himself or by the health personnel; doctor, nurse, pharmacist. The EHS recent guidelines [28], recommends to recheck blood pressure at one to two monthly intervals after initiation of therapy until blood pressure remains at target level for two consecutive visits then recheck at 3 to 6 month intervals depending upon the risk profile. Frequency of office visits depends upon: comorbidities such as heart failure; coronary diseases, CKD and/or diabetes; and for the need of laboratory tests. Lifestyle modifications should be reviewed, reemphasized and documented annually. Treatment and follow- up should continue indefinitely (Figure 6).
Role of pharmaceutical industry
Drug companies provide financial support to develop and implement patients and health workers (physicians, pharmacists, nurses) education programs, to produce more generic and off patent medicines and establish specialized hypertension clinics. Drug industry in collaboration with the EHS is sponsoring, besides the education programs and hypertension clinics, a number of activities which include research projects such as calibration and assessing the validity of blood pressure measuring devices in hospitals, doctors offices and pharmacies. Another project is correlation of AOBP with central aortic pressures and indices of arterial stiffness. Also industry is financing blood pressure screening service at metro stations in Greater Cairo area and activities of the World Hypertension Day (Figure 7).
What Do We Need For The Future?
More education and new epidemiologic data
Hypertension is either undetected or poorly managed with problems of over and under-diagnosis. The Egyptian Hypertension Society (EHS) actively engaged in public and physicians programs stressing the silent nature of hypertension, the need to check blood pressure periodically to make the diagnosis, there is no cure from established essential hypertension, therefore pharmacologic treatment should continue indefinitely.
The EHS needs the support of health authorities, social organizations and drug industry to expand its education programs.
New epidemiologic studies are needed to identify the magnitude of hypertension problem in the country and trends in blood pressure. Finding reasons for difference in prevalence of hypertension among individuals of the same ethnic origin, which we reported in the Egyptian National Hypertension Project (NHP 1991-1994) [29], will help clarify some hypertension risk factors. The role of emerging dietary risk factors (e.g. sugar & fat) and of environmental pollution (air and noise) require further investigations. Magnitude and reasons for lack of drug adherence and cost effectiveness of aggressive management of hypertension in a developing country like Egypt can be investigated in future epidemiologic surveys.
National programs for hypertension control
• EHS together with health authorities should work together to develop and disseminate an update of the EHS guidelines and finding ways of translating guidelines into clinical practice. More effective public awareness programs through social media, internet, press and TV should outline the components of healthy lifestyle and need for regular checking blood pressure.
• Salt reduction campaign through media and governments legislations, limiting salt content of food. Food labeling and making healthy low salt foods readily available and affordable.
• An up-to-date list of essential drugs should be prepared and generic prescriptions should be encouraged by the EHS and health authorities. Clinicians should prescribe generic medicines if possible, rather than expensive brand-named medications.
• Routine opportunistic screening should be encouraged with establishing blood pressure checking stations in malls and metro stations.
• In order to continue and maintain their services, the present EHS specialized hypertension clinics require continued support from drug industry and health authorities.
• A successful blood pressure screening program (30) should include 1. Training to accurately measure blood pressure; 2. Use of accurate equipment (blood pressure devices) - semi-automated devices are recommended; 3. appropriate interpretations of blood pressure readings: e.g. blood pressure of 140-170/90-95 mmHg will require follow-up within a few weeks, if more than 180 mmHg, follow-up as soon as possible by a medical doctor; 4. follow-up instructions can be provided at blood pressure checking stations as posters or other forms of printed material.
• The EHS is developing a community based blood pressure screening program at metro stations run by young doctors.
• Ensuring access and supply of inexpensive medicines and promoting local manufacturing of generic medicines.
More involvement of pharmacists & nurses
Pharmacists and nurses education is important. The EHS is planning pharmacists' education program, measuring and monitoring blood pressure, patient education, paying reminder phone calls for drug intake and office appointments. Nurses lead blood pressure screening in community, worksite, schools and other settings.
Community based blood pressure screening programs
Medical societies and health authorities should develop and encourage blood pressure screening in all health facilities, sporting and social clubs, metro stations and shopping malls. Media, press, TV, radio and internet should increase public awareness and the need for checking blood pressure.
New management tools
The efficacy and cost effectiveness of hypertension new diagnostic and management tools need to be tested in the community setting. Electronic health records (EHR), automated office blood pressure (AOBP) measurement [30,31], telemedicine and home blood pressure tele-monitoring [32] are new tools, their role in management of patients in our community is not defined. EHR has been shown to improve the quality of care as a result of having health information immediately available at all times. AOBP has proved to have greater accuracy and consistency than manual blood pressure. AOBP has been recommended by the recent hypertension guidelines as the diagnostic method of choice to confirm the presence of hypertension.
Telemedicine and in particular home blood pressure telemonitoring (HBPT) is a promising in blood pressure control [33]. HBPT consists of automatic blood pressure data transmission from the patient's home to the doctor's office. HBPT showed clear benefit in terms of greater blood pressure reduction, but the overall costs were significantly high (Figure 8).
References
- Krause T, Lovibond K, Caulfield M, McCormack T, Williams B. Guideline Development Group. Management of hypertension: summary of NICE guidance. BMJ. 2011; 343: d4891. Ref.: https://goo.gl/y2c3AK
- Gabb GM, Mangoni AA, Anderson CS, Cowley D, Dowden JS, et al. Guideline for the diagnosis and management of hypertension in adults - 2016. Med J Aust. 2016; 25: 85-89. Ref.: https://goo.gl/emqVJi
- Leung AA, Daskalopoulou SS, Dasgupta K, McBrien K, Butalia S, et al. Hypertension Canada. Hypertension Canada's 2017 Guidelines for Diagnosis, Risk Assessment, Prevention, and Treatment of Hypertension in Adults. Can J Cardiol. 2017; 33: 557-576. Ref.: https://goo.gl/yNszCA
- Garry LR Jennings, Touyz RM. Hypertension Guidelines. More Challenges Highlighted by Europe. Hypertension. 2013; 62: 660-665. Ref.: https://goo.gl/Xxr8da
- Myers MG. Replacing manual sphygmomanometers with automated blood pressure measurement in routine clinical practice. Clin Exp Pharmacol Physiol. 2014; 41: 46-53. Ref.: https://goo.gl/bHMPu5
- World Health Organization. Affordable technology, blood pressure measuring devices for low resource settings. Report 1-26. Geneva, Switzerland. World Health Organization 2005; Ref.: https://goo.gl/Fru7Me
- Campbell NR, Berbari AE, Cloutier L, Gelfer M, Kenerson JG, et al. Policy statement of the world hypertension league on noninvasive blood pressure measurement devices and blood pressure measurement in the clinical or community setting. J Clin Hypertens (Greenwich). 2014; 16: 320-322. Ref.: https://goo.gl/g2EEW3
- Myers MG, Kaczorowski J, Paterson JM, Dolovich L, Tu K. Thresholds for Diagnosing Hypertension Based on Automated Office Blood Pressure Measurements and Cardiovascular Risk. Hypertension. 2015; 66: 489-495. Ref.: https://goo.gl/TNGyKD
- Whelton PK, Carey RM, Aronow WS, Casey E, Collins KJ, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults. A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. Hypertension. 2018; 71: 1269-1324. Ref.: https://goo.gl/CV78aL
- SPRINT Research Group, Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, et al. A Randomized Trial of Intensive versus Standard Blood-Pressure Control. N Engl J Med. 2015; 373: 2103-2116. Ref.: https://goo.gl/bD9psw
- Mueller Paul S. Clinic-based BP Measurement is inaccurate for diagnosing hypertension. J Watch Gen Med. 2011; Ref.: https://goo.gl/1NegsB
- Myers MG, Godwin M, Dawes M, Kiss A, Tobe SW, et al. Measurement of blood pressure in the office. Recognizing the problem and proposing the solution. Hypertension. 2010; 55: 195–200. Ref.: https://goo.gl/7A1W2A
- Hodgkinson J, Mant J, Martin U, Guo B, Hobbs FD, et al. Relative effectiveness of clinic and home blood pressure monitoring compared with ambulatory blood pressure monitoring in diagnosis of hypertension: systematic review. BMJ. 2011; 342: d3621. Ref.: https://goo.gl/XkSQ6K
- Padfield PL. Reduction of cardiovascular morbidity and mortality in the third world: the importance of accurate blood pressure measurement. Hypertension. 2010; 56: 1038–1039. Ref.: https://goo.gl/F6ZFdp
- Mulrow PJ. Hypertension: a worldwide epidemic. In: Izzo JL, Black HR, Goodfriend TL, editors. Hypertension primer: the essentials of high blood pressure. 2nd ed. Baltimore: Williams and Wilkins; 1999; 271–273. Ref.: https://goo.gl/2HsPKb
- Myers MG, Valdivieso M, Kiss A. Use of automated office blood pressure measurement to reduce the white coat response. J Hypertens. 2009; 27: 280–286. Ref.: https://goo.gl/xhiU4n
- Graves JW, Nash C, Burger K, Bailey K, Sheps SG. Clinical decision-making in hypertension using an automated (BpTRU) measurement device. J Hum Hypertens. 2003; 17: 823–827. Ref.: https://goo.gl/PsJsSv
- Mendis S, Lindholm LH, Mancia G, Whitworth J, Alderman M, et al. World Health Organization (WHO) and International Society of Hypertension (ISH) risk prediction charts: assessment of cardiovascular risk for prevention and control of cardiovascular disease in low and middle-income countries . J Hypertens. 2007; 25: 1578-1582. Ref.: https://goo.gl/upQ2Mp
- The Cochrane collaboration 2012.
- Nielsen JØ, Shrestha AD, Neupane D, Kallestrup P. Non-adherence to anti-hypertensive medication in low- and middle-income countries: a systematic review and meta-analysis of 92443 subjects. J Hum Hypertens. 2017; 31: 14-21. Ref.: https://goo.gl/xngY8c
- Ibrahim MM. Discontinuation rates of antihypertensive drugs among Egyptian patients and physician survey. Unpublished observations. 1998.
- Vrijens B1, Vincze G, Kristanto P, Urquhart J, Burnier M. Adherence to prescribed antihypertensive drug treatments: longitudinal study of electronically compiled dosing histories. BMJ. 2008; 336: 1114-1117. Ref.: https://goo.gl/ojermR
- Campbell NR, Lackland DT, Chockalingam A, Lisheng L, Harrap SB, et al. The International Society of Hypertension and World Hypertension League call on governments, nongovernmental organizations and the food industry to work to reduce dietary sodium. J Hypertens. 2014; 32: 446-447. Ref.: https://goo.gl/g6Veoo
- Himmelfarb CR, Commodore-Mensah Y, Hill MN. Expanding the Role of Nurses to Improve Hypertension Care and Control Globally Ann Glob Health. 2016; 82: 243-253. Ref.: https://goo.gl/QzHPJJ
- Carter BL, Bosworth HB, Green BB. The hypertension team: the role of the pharmacist, nurse, and teamwork in hypertension therapy. J Clin Hypertens (Greenwich). 2012; 14: 51-65. Ref.: https://goo.gl/HQVz6r
- WHO | Health systems financing: the path to universal coverage. 2010; Ref.: https://goo.gl/qkLvhX
- World Health Organization Spending on Health: a global overview. Fact Sheet no. 319. 2012; Ref.: https://goo.gl/SCfuV7
- Ibrahim MM. The Egyptian hypertension society: Egyptian hypertension guidelines. Egyptian Heart Journal. 2014; 66: 79-132. Ref.: https://goo.gl/u95UKM
- Ibrahim MM, Rizk H, Appel LJ, el Aroussy W, Helmy S, et al. Hypertension prevalence, awareness, treatment, and control in Egypt. Results from the Egyptian National Hypertension Project (NHP). NHP Invest Team. Hypertens.1995; 26 (6 Pt 1): 886–890. Ref.: https://goo.gl/DxWCUk
- Myers MG. Replacing manual sphygmomanometers with automated blood pressure measurement in routine clinical practice. Clin Exp Pharmacol Physiol. 2014; 41: 46-53. Ref.: https://goo.gl/AC4eKW
- Campbell NR, Berbari AE, Cloutier L, Gelfer M, Kenerson JG, et al. Policy statement of the world hypertension league on noninvasive blood pressure measurement devices and blood pressure measurement in the clinical or community setting. J Clin Hypertens (Greenwich). 2014; 16: 320-322. Ref.: https://goo.gl/24hxGF
- Mboni S, Ferrari R. The role of telemedicine in hypertension management: focus on blood pressure telemonitoring. Curr Hypertens Rep. 2015; 17: 535. Ref.: https://goo.gl/1vh73m
- Omboni S, Gazzola T, Carabelli G, Parati G. Clinical usefulness and cost effectiveness of home blood pressure telemonitoring: Meta-analysis of randomized controlled studies. J Hypertens. 2013; 31: 455–468. Ref.: https://goo.gl/iuUEgy