More Information
Submitted: November 26, 2022 | Approved: December 05, 2022 | Published: December 06, 2022
How to cite this article: Christou V, Karataraki FZ, Eid O, Eid R, Moutiris JA. Prevalence of Hypertension in patients with chronic Coronary Artery Disease in Cyprus. Ann Clin Hypertens. 2022; 6: 015-019.
DOI: 10.29328/journal.ach.1001031
Copyright License: © 2022 Christou V, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Coronary Artery Disease; Hypertension; Cardiology; Prevalence; Secondary prevention; Cyprus
Prevalence of Hypertension in patients with chronic Coronary Artery Disease in Cyprus
Vasiliki Christou, Fedra Zoi Karataraki, Omar Eid, Rasha Eid and Joseph A Moutiris*
Department of Cardiology, Medical School, University of Nicosia, Paphos General Hospital, Cyprus
*Address for Correspondence: Joseph A Moutiris, Professor, Department of Cardiology, Medical School, University of Nicosia, Paphos General Hospital, Paphos 8100, Cyprus, Email: [email protected]
Coronary Artery Disease (CAD) is the most common type of heart disease and a major cause of mortality worldwide. This study highlights the significance of hypertension as a risk factor in patients with CAD and compares its prevalence to those of EUROASPIRE IV (EUS-IV), ESC Atlas of Cardiology (Atlas) and Cyprus Survey of Coronary Heart Disease of 2006 (CY-2006).
A retrospective, observational study was conducted, by the Registry of Cyprus Heart Survey, where 375 individuals with chronic CAD were examined in Nicosia General Hospital Cardiology Clinics, between the years 2011 and 2014. Their medical history regarding hypertension was noted and the data was analyzed using Microsoft Excel software.
The total prevalence of hypertension, based on the past medical history of the patients was 59%.
Out of these, 52% were found to have elevated blood pressure on their visit to the Cardiology Clinic. The total mean systolic blood pressure amongst the study group was 136 mmHg, with no significant differences between males and females (136 mmHg and 134 mmHg respectively).
The findings of the present study are the same compared to those of the CY-2006 (52% both), but slightly higher than the findings of EUS-IV (52% vs. 42.7%) and significantly higher than those recorded in the Atlas (52% vs. 24.8%).
The results show that there is still much potential to improve hypertension management in patients with established CAD.
Coronary Artery Disease (CAD) is the most common and most fatal heart condition, affecting 20.1 million adults aged 20 and above and causing 17.9 million deaths worldwide, annually [1-3]. Specifically, in 2020, 382,820 people died because of Coronary Artery Disease, based on the latest statistics published by CDC [1].
CAD is caused when the oxygen needs of the myocardium are not met, due to inadequate blood supply. The major underlying mechanism is the build-up of lipid-rich plaques in the coronary arteries. This leads to progressive vascular obstruction, impaired perfusion of the myocardium, ischemia, and gradual cardiac cell death, resulting eventually in acute coronary syndromes [4,5].
Coronary artery disease is a chronic disease that develops over the years, and it might go unnoticed until the first cardiovascular event. One major contributing factor to the disease is hypertension [4]. Hypertension is defined as more than one reading of blood pressure (BP) above 140/90 mmHg [6] and it is further subclassified into 6 categories, starting from optimal (systolic BP < 120, diastolic BP < 80) and reaching grade 3 hypertension (systolic BP > 180, diastolic BP > 110). More details about the classification can be found in Table 1.
| Table 1: Classification of clinical hypertension. | |||
| Category | Systolic (mmHg) | Diastolic (mmHg) | |
| Optimal | < 120 | And/or | < 80 |
| Normal | 120-129 | And/or | 80-84 |
| High normal | 130-139 | And/or | 85-89 |
| Grade 1 Hypertension | 140-159 | And/or | 90-99 |
| Grade 2 Hypertension | 160-179 | And/or | 100-109 |
| Grade 3 Hypertension | > 180 | And/or | > 110 |
| Isolated Systolic Hypertension | > 140 | and | < 90 |
An estimated 1.28 billion adults aged 30 - 79 years worldwide have hypertension [7], while, in the Cypriot population the prevalence of hypertension is 31.2% in males and 21.3% in females (26% on average), according to WHO [8].
The relationship between hypertension and CAD is characterized by complicated pathophysiological mechanisms. Hypertension is responsible for endothelial damage thus, accelerating the creation of atherosclerotic plaques, before destabilizing them [9]. Furthermore, hypertension causes left ventricular and arterial hypertrophy, which subsequently increases ventricular and arterial wall stiffness [9]. This increases the myocardial oxygen demand, which cannot be satisfied since coronary perfusion pressure falls, thus precipitating myocardial ischemia. Lastly, hypertension causes arterial stiffness which leads to increased blood backflow, which further intensifies hypertension. This vicious cycle deteriorates further the already aggravated condition of the heart [9,10].
The aim of this study is to highlight the significance of hypertension as a risk factor in patients with CAD, using data received from the Cyprus Heart Survey registry. Furthermore, the findings are compared to those of EUROASPIRE IV, which addressed secondary prevention of CAD across 24 European countries, and the data given by the ESC Atlas of Cardiology in 2019. Finally, the results are also compared to those announced earlier by the Cyprus Survey in 2006, a study that also assessed the prevalence of coronary risk factors in patients with previous coronary events.
Study design
A retrospective, observational study was created with data extracted from the Registry of Cyprus Heart Survey. The study consisted of 375 consecutive individuals with a background of CAD who were examined in Nicosia General Hospital Cardiology Clinics between the years 2011 and 2014. The study aimed at the detection of hypertension, past, and current.
Patient selection and subgroups
The eligibility of a patient was determined based on the history of CAD or previous hospitalization for coronary incidents or interventions. Patients from both genders with ages varying from 32 to 92 were selected and each one of the 375 individuals was interviewed by cardiology specialists and a focused history regarding hypertension was obtained.
The prevalence of hypertension in the study population was determined based on the previous and current history of hypertension at a specific time period, which is either well- or poorly controlled. Particularly, at the time of the interview, the assessment of their past medical history regarding hypertension was done using the questions “Have you ever had a problem with your blood pressure?”, “Have you been taking medication for high blood pressure?” and “Has your blood pressure ever been elevated in the past?”, before proceeding to the measurement of the patient’s blood pressure on site.
For blood pressure measurement, the consultants used automatic digital sphygmomanometers on the patient’s right arm. All the patients had their blood pressure recorded three times, in the sitting position, and the mean value of the three recordings was considered for the statistical analysis.
For data collection and analysis, the patients were divided into specific subgroups as follows: (i) males on antihypertensive medications, (ii) females on antihypertensive medications, (iii) males with well-controlled hypertension at interview (systolic BP< 140 mmHg), (iv) males with uncontrolled hypertension at interview (systolic BP > 140 mmHg), (v) females with well-controlled hypertension at interview and (vi) females with poorly controlled hypertension at interview, as seen in Table 2.
| Table 2: Patients with a history of hypertension and controlled/uncontrolled hypertension. | |||
| Characteristics | Patients on antihypertensive medication, N = 284 (75.7%) |
Patients with well-controlled hypertension on examination, N = 216 (58%) |
Patients with uncontrolled hypertension on examination, N = 159 (42%) |
| Sex, n (%) | |||
| Female | 32 (73%) | 30 (68%) | 13 (29.5%) |
| Male | 252 (76%) | 186 (56%) | 146 (44%) |
| Age in years | |||
| Total mean (SD) | 66.7 (10.3) | 66.5 (10.6) | 68 (8.5) |
| Female mean (SD) | 70 (10.6) | 69 (10.1) | 76 (7.8) |
| Male mean (SD) | 66.2 (10.2) | 66 (10.6) | 67.4 (8.2) |
Antihypertensive medications are defined as the intake of either Angiotensin-converting enzyme (ACE) inhibitors, Angiotensin Receptor blockers (ARBs), or β-blockers.
Statistical analysis
Categorical data, such as gender and age groups, were expressed as absolute numbers and percentages. Continuous variables, such as the systolic BP (SBP) and diastolic (DBP) were described as mean and standard deviation (SD).
The latter set of data was analyzed using Microsoft 365 Excel. Initially, the percentage of patients that had on their on-site examination SBP less than 140 mmHg and SBP greater than 140 mmHg, was calculated.
Additionally, each gender population was segregated, and based on each individual’s SBP and DBP values, the percentage of male, female and total patients that correspond to the different grades of hypertension was estimated, as seen in Table 3.
| Table 3: Classification based on the grade of hypertension. | ||||||||
| Category | Systolic | Total (%) | Female (%) | Male (%) | Diastolic | Total (%) | Female (%) | Male (%) |
| Optimal | < 120 | 12 | 11.3 | 12.3 | And/or < 80 | 32 | 48 | 30 |
| Normal | 120-129 | 16.5 | 18 | 16.3 | And/or 80-84 | 32.2 | 32 | 32.3 |
| High normal | 130-139 | 29 | 38.6 | 27.4 | And/or 85-89 | 16.5 | 16 | 16.6 |
| Grade 1 Hypertension | 140-159 | 33 | 13.6 | 36 | And/or 90-99 | 17 | 4,5 | 18.4 |
| Grade 2 Hypertension | 160-179 | 7 | 16 | 5.7 | And/or 100-109 | 2 | 0 | 2.4 |
| Grade 3 Hypertension | > 180 | 2.4 | 0 | 2,7 | And/or > 110 | 0 | 0 | 0 |
| Isolated Systolic Hypertension | > 140 | 19 | 20 | 19 | And < 90 | |||
Finally, the percentage of patients who were on either ACE inhibitors, ARBs, or β-blockers treatment was calculated, based on the information gathered during the consultations.
Outcome measures
The main outcome measures were the estimation of the total prevalence of hypertension in the patients and the assessment of whether the secondary prevention guidelines of the ESC are appropriately met.
The study population included 375 individuals of whom 12% were females. On presentation to the clinic, the mean systolic blood pressure was 136 mmHg (±17), with no significant differences between males and females, with 136 mmHg (±17) and 134 mmHg (±17.2), respectively. In addition, the percentage of patients who had SBP > 140 mmHg was 42% (females 29%, males 44%).
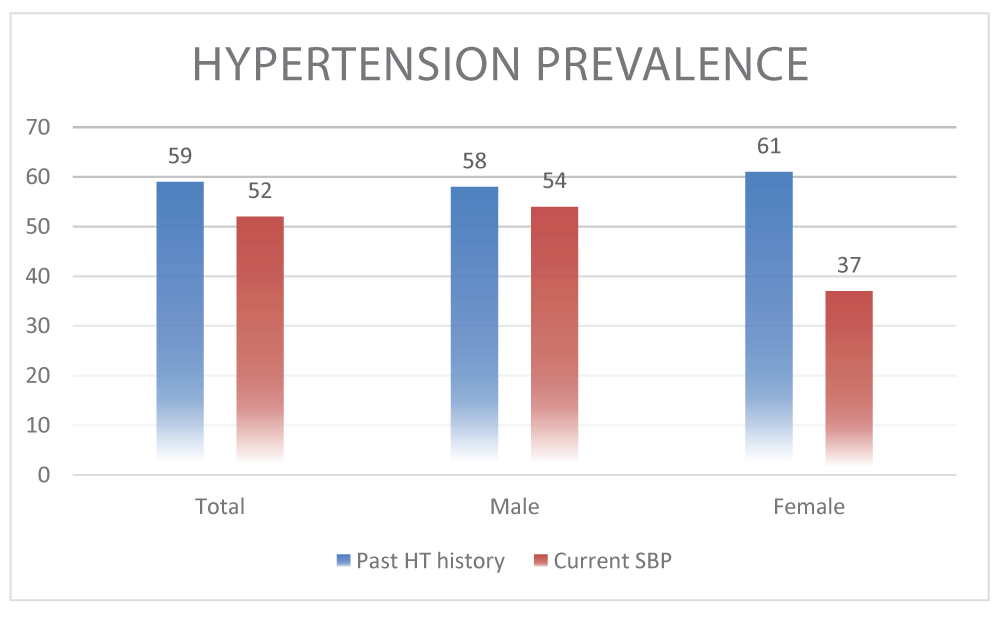
223 patients (prevalence 59%) had a previous history of hypertension (196 males, 27 females). On their visit to the Cardiology Clinic, on average 9 years after the first event, 116 patients (106 males and 10 females) of these 223 (prevalence 52%), were found to have abnormally elevated blood pressure (Figure 1).
Figure 1: Prevalence of hypertension: past history vs. current examination.
Additionally, 43 patients (40 males, 3 females) of the 125 who did not have a prior history of hypertension, were found on presentation to the clinic to have abnormally elevated BP (prevalence 28%).
Last but not least, the patients who were on cardioprotective/antihypertensive treatment (either ACEIs/ARBs or B Blockers) at the time of the interview were 75.7%. More specifically 59.2% were on ACEIs, 63.2% were on β- blockers, and 46.7% were on both.
omparison of Cyprus Heart Survey 2014 to EUROASPIRE IV
Comparing the results of the Cyprus Heart Survey to the ones of EUROASPIRE IV, the prevalence of hypertension in the EUS-IV study was 42.7%, much lower than the 52% of the present study. Regarding the prevalence of hypertension according to gender, in females, it was found to be 44%, compared to 37%, and in males 42%, compared to 54%, in EUS-IV and Cyprus Heart Survey, respectively [11].
Furthermore, the number of patients in the two studies, who were on antihypertensive therapy was similar. In the EUROASPIRE IV, 78.1% of the total population was on antihypertensive treatment [11], while 75.7% of the total patients enrolled in the Cyprus Registry were taking antihypertensive medications at the time of the interview.
Nonetheless, the target goal of BP < 140/90 mmHg was achieved in 48% of the patients in the Cyprus Heart Survey, compared to 40% of the Euroaspire IV population. The great diversity among the European populations was perhaps the reason for the lower target goal achievement in the EUROASPIRE IV study.
In summary, the Cyprus Heart Survey has noted a higher prevalence of hypertension by 21%, a lower percentage of patients on antihypertensive medication by 3.8% and a higher percentage of patients achieving their BP target by 16.6%, compared to the EUS-IV.
Comparison of Cyprus heart survey 2014 to European society of cardiology Atlas 2019
According to the European Society of Cardiology in 2019, the total prevalence of hypertension in 56 European countries, including Cyprus, appeared to be 24.8%, with median rates of 22.3% for females and 27.0% for males [12]. This difference between our study and ESC Atlas is attributed to the greater sample size (375 vs. 10 mil.) of the Atlas.
It is an admirable fact that the results derived from Atlas were compatible with the ones received from our study, highlighting the lower prevalence of hypertension in the female population in the two studies. Although no further information regarding the reason for that difference has been obtained, the similarity in the results shows that there is definitely a correlation between the two genders and the progression of hypertension, making it an interesting topic for further research.
Comparison of Cyprus heart survey 2014 to Cyprus survey 2006
The results obtained from the Cyprus Survey in 2006 showed a total prevalence of hypertension of 52% on the visit to the clinic that took place approximately 1.6 years after the event [13,14], the same as the Cyprus Heart survey 2014. This reveals that there has been no noticeable improvement in the management of hypertension over a period of 8 years.
Limitations
The Cyprus CAD study presents a few limitations. First of all, the sample size of the population studied was small. Additionally, the lack of information regarding further follow-up resulted in a gap of insight into the long-term progression of the hypertension status for each coronary patient. Building upon that, we cannot account for what percentage of those who remained hypertensive, is attributed to the lack of adherence to the medication or the lifestyle modifications. The main strength of the study is that despite the restricted sample size, the Registry of Cyprus withholds records from all the public hospitals of the country, making the results reliable and representative of the Cypriot population, which is less than one million. Furthermore, the BP monitoring was done by highly experienced personnel, who utilized modern and accurate sphygmomanometers, resulting in reliable quality information.
After analyzing and comparing the results of our study to those of EUROASPIRE IV, ESC Atlas 2019, and the Cyprus survey of 2006, it is observed that although they are in accordance, there has been no improvement noted in hypertension management in the island of Cyprus. Therefore, the weight of uncontrolled hypertension remains heavy, and refining the control of hypertension is a strategic initiative of worldwide proportions, in order to decrease the cardiovascular disease burden. Closing the gap requires small and feasible management plans to ensure appropriate diagnosis, optimal treatment, and patient adherence.
- CDC. Heart disease Facts. Centers for Disease Control and Prevention. 2021. https://www.cdc.gov/heartdisease/facts.htm
- World Health Organization. Cardiovascular diseases. World Health Organisation. 2022. https://www.who.int/health-topics/cardiovascular-diseases#tab=tab_1
- Brown JC, Gerhardt TE, Kwon E. Risk Factors for Coronary Artery Disease. 2022 Jun 5. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 32119297.
- Mayo Clinic. Coronary artery disease. Mayo Clinic. 2020. https://www.mayoclinic.org/diseases-conditions/coronary-artery-disease/symptoms-causes/syc-20350613
- Mayo Clinic. Acute coronary syndrome - Symptoms and causes. 2019. https://www.mayoclinic.org/diseases-conditions/acute-coronary-syndrome/symptoms-causes/syc-20352136
- NICE. Recommendations. Hypertension in adults: diagnosis and management. Guidance. NICE. Nice.org.uk. NICE; 2019. https://www.nice.org.uk/guidance/ng136/chapter/Recommendations#diagnosing-hypertension
- World Health Organization. Hypertension. Who.int. World Health Organization: WHO; 2021. https://www.who.int/news-room/fact-sheets/detail/hypertension
- Kypris L. Country report Cyprus. Structure of health care Country report of Cyprus. https://www.escardio.org/static-file/Escardio/Subspecialty/EAPC/Country%20of%20the%20month/Documents/cyprus-country-of-the-month-full-report.pdf
- Escobar E. Hypertension and coronary heart disease. J Hum Hypertens. 2002 Mar;16 Suppl 1:S61-3. doi: 10.1038/sj.jhh.1001345. PMID: 11986897.
- Weber T, Lang I, Zweiker R, Horn S, Wenzel RR, Watschinger B, Slany J, Eber B, Roithinger FX, Metzler B. Hypertension and coronary artery disease: epidemiology, physiology, effects of treatment, and recommendations : A joint scientific statement from the Austrian Society of Cardiology and the Austrian Society of Hypertension. Wien Klin Wochenschr. 2016 Jul;128(13-14):467-79. doi: 10.1007/s00508-016-0998-5. Epub 2016 Jun 9. PMID: 27278135.
- Kotseva K, Wood D, De Bacquer D, De Backer G, Rydén L, Jennings C, Gyberg V, Amouyel P, Bruthans J, Castro Conde A, Cífková R, Deckers JW, De Sutter J, Dilic M, Dolzhenko M, Erglis A, Fras Z, Gaita D, Gotcheva N, Goudevenos J, Heuschmann P, Laucevicius A, Lehto S, Lovic D, Miličić D, Moore D, Nicolaides E, Oganov R, Pajak A, Pogosova N, Reiner Z, Stagmo M, Störk S, Tokgözoğlu L, Vulic D; EUROASPIRE Investigators. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur J Prev Cardiol. 2016 Apr;23(6):636-48. doi: 10.1177/2047487315569401. Epub 2015 Feb 16. PMID: 25687109.
- Atlas Writing Group; ESC Atlas of Cardiology is a compendium of cardiovascular statistics compiled by the European Heart Agency, a department of the European Society of Cardiology.; Developed in collaboration with the national societies of the European Society of Cardiology member countries, Timmis A, Townsend N, Gale CP, Torbica A, Lettino M, Petersen SE, Mossialos EA, Maggioni AP, Kazakiewicz D, May HT, De Smedt D, Flather M, Zuhlke L, Beltrame JF, Huculeci R, Tavazzi L, Hindricks G, Bax J, Casadei B, Achenbach S, Wright L, Vardas P. European Society of Cardiology: Cardiovascular Disease Statistics 2019 (Executive Summary). Eur Heart J Qual Care Clin Outcomes. 2020 Jan 1;6(1):7-9. doi: 10.1093/ehjqcco/qcz065. PMID: 31957796.
- Moutiris J, Mavrommatis P, Ioannides M, Nicolaides E, Tryfonas A, Minas M. Cyprus survey of Coronary Heart Disease: Risk factors and treatment in patients with history of MI and PCI or CABG surgery. European Heart Journal. 2006; 27(6):658–8.
- Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, Kahan T, Mahfoud F, Redon J, Ruilope L, Zanchetti A, Kerins M, Kjeldsen SE, Kreutz R, Laurent S, Lip GYH, McManus R, Narkiewicz K, Ruschitzka F, Schmieder RE, Shlyakhto E, Tsioufis C, Aboyans V, Desormais I; Authors/Task Force Members:. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018 Oct;36(10):1953-2041. doi: 10.1097/HJH.0000000000001940. Erratum in: J Hypertens. 2019 Jan;37(1):226. PMID: 30234752.