More Information
Submitted: August 17, 2023 | Approved: September 15, 2023 | Published: September 19, 2023
How to cite this article: OMONIJO A, OLOWOYO P, IBRAHIM AO, AGBOOLA SM, AJETUNMOBI OA, et al. Relationship between the Level of Spirituality and Blood Pressure Control among Adult Hypertensive Patients in a Southwestern Community in Nigeria. Ann Clin Hypertens. 2023; 7: 004-012.
DOI: 10.29328/journal.ach.1001034
Copyright License: © 2023 OMONIJO A, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Keywords: Spirituality; Blood pressure control; Hypertension
Relationship between the Level of Spirituality and Blood Pressure Control among Adult Hypertensive Patients in a Southwestern Community in Nigeria
Adetunji OMONIJO1*, Paul OLOWOYO2, Azeez Oyemomi IBRAHIM3, Segun Matthew AGBOOLA3, Oluwaserimi Adewumi AJETUNMOBI3, Temitope Moronkeji OLANREWAJU1 and Adejumoke Oluwatosin OMONIJO4
1Department of Family Medicine, Federal Teaching Hospital Ido-Ekiti, Ekiti State
2Department of Internal Medicine, Afe Babalola University, Ado-Ekiti, Ekiti State, Nigeria
3Department of Family Medicine, Afe Babalola University, Ado-Ekiti, Ekiti State, Nigeria
4Department of Animal and Environmental Biology, Federal University Oye-Ekiti, Ekiti State, Nigeria
*Address for Correspondence: Adetunji OMONIJO, Department of Family Medicine, Federal Teaching Hospital, Ido-Eki, Ekiti State, Nigeria, Email: [email protected]
Background: Spirituality has been strongly associated with good blood pressure control as it forms a strong coping mechanism in hypertensive patients. This hospital-based cross-sectional study was done to determine the relationship between spirituality and blood pressure control among adult hypertensive patients in rural Southwestern Nigeria to achieve good blood pressure control.
Method: The selection was done by systematic random sampling technique. Socio-demographic and clinical information were obtained through semi-structured interviewer-administered questionnaires. The level of spirituality was assessed using the Spiritual Perspective Scale. Data were analysed using the Statistical Package for Social Sciences version 20.0. Statistical significance was set at p ≤ 0.05.
Results: The mean age of the respondents was 61.1 ± 11.1 years. More than half (52.6%) had a high level of spirituality and more than two-thirds (67.1%) of respondents had controlled blood pressure. Respondents with a high level of spirituality were 4.76 times more likely to have good blood pressure control {p < 0.001, 95% CI (1.05-14.99)} than those with a low level of spirituality.
Conclusion: Proper understanding and effective utilization of this relationship will assist health professionals and researchers in the appropriate integration of this concept into patients’ holistic care with the aim of achieving better blood pressure control among hypertensive patients.
Hypertension and its associated complications have become a common and important global public health challenge of the 21st century [1-3]. Hypertension is a major risk factor and a powerful predictor of cardiovascular morbidity and mortality [1,4]. The global prevalence of hypertension has been increasing. For instance, in the year 2000, the world was estimated to have close to 1 billion people with hypertension with a prevalence rate of 26.4% and this has been projected to increase to 1.56 billion affected individuals with a prevalence rate of 29.2% in 2025, the population burden being greater in developing countries [2,5]. In Africa, blood pressure control rates were uniformly low and often did not exceed 45% of the hypertensive population [6]. A hospital-based study in Port-Harcourt, Nigeria shows that good hypertension control could only be achieved for just 24.2% of the patients seen in the clinic [7]. According to a community-based study among an urban population in Zaria, Nigeria the hypertension control rate was only 12.4% among patients who have been on antihypertensive medications for over 3 months [8]. These gloomy statistics call for urgent action, especially as the WHO has projected a further 24% increase in the prevalence of non-communicable diseases in Nigeria, in the next 10 years [6]. Worldwide, there has been a systematic introduction of the concept of spirituality into the medical field with a growing interest in the possible health benefits as a result of having a spiritual belief and following a religious lifestyle [9].
Spirituality can be defined as “the aspect of humanity that refers to the way individuals seek and express meaning and purpose and the way they experience their connectedness to the moment, to self, to others, to nature, and the significant or sacred” [10] Spirituality has been found to play vital roles in health through disease detection and treatment compliance, beliefs that conflict with medical care, medical decision making and spiritual struggles that create stress and impair health outcome [11]. Specifically, it has been noted as an essential factor influencing the health-related quality of life of chronically ill patients due to its integration into positive thoughts and health behaviors, as well as healthy coping styles which alleviate the perceived overwhelming persistent situation [12,13].
Spirituality has been associated with good blood pressure control in hypertensive patients [14]. The importance of addressing spirituality in hypertension like in other chronic diseases is indicated in several studies [8,13,15]. Spirituality is important to hypertensive patients, and some patients have indicated that they use their spirituality for coping and disease management [16]. In a study conducted by Kretchy, et al. [8] findings revealed that participants with a high level of spirituality and religious participation had significantly lower diastolic and systolic blood pressure than their counterparts with a low level of spirituality (77.8 vs. 84.7 mmHg and 137.2 vs. 149.5 mmHg, respectively) after adjusting for demographic, sociocultural, and psychological variables [8]. Studies have also revealed that people who engaged in spiritual activities had lower levels of cortisol (a biological marker of stress) attenuation of neural responses to stress responsivity, regulation of emotion during exposure to stress, prevention and reduction of stress-related psychopathology, good lipid profiles, good glucose control, and a functional immune system [16-18]. There is a paucity of studies on the relationship between spirituality and blood pressure control in Nigeria.
This study is designed to determine the role of spirituality in the control of blood pressure among adult hypertensive patients
Study area/study design/population
The hospital-based descriptive cross-sectional study was conducted among adult hypertensive patients aged 18 years and above attending the Family Medicine Clinic of Federal Teaching Hospital, Ido-Ekiti (FETHI) in rural Southwest Nigeria. The study was conducted over sixteen (16) weeks from April to July 2017 during which a total of 1,986 hypertensive patients were encountered.
Sample size determination
The sample size was calculated using the formula for estimating proportions in a cross-sectional study: n = z2 pq/d2 (For population > 10,000) [19] and nf = n/1+ (n/N) (For population < 10,000) [19].
Where:
n = the minimum sample size when the population is more than 10,000.
nf = the minimum sample size when the population is less than 10,000.
N = the estimate of study population size in a given year, i.e. adult hypertensive patients who attended the Family Medicine Clinic of Federal Teaching Hospital in 2015.
(N = 4,800).
zα = the level of confidence (The standard normal deviation set at 1.96 which corresponds to the 95% confidence level obtained from the standard statistical table of normal distribution.
p = Estimated prevalence of medication adherence among hypertensive patients in a given population, (using 37.2%, which was the prevalence of hypertension among hypertensive patients at a tertiary hospital, in rural Southeast Nigeria) [20].
q = 1–p.
d = Degree of accuracy desired usually set at 0.05
The minimum sample size was 334 respondents. However, to allow for non-responses during recruitment, a non-response value of 10% (33) was added to the minimum sample size (nf). This gave a minimum sample size of 367 respondents. Hence, 367 respondents were used for the study.
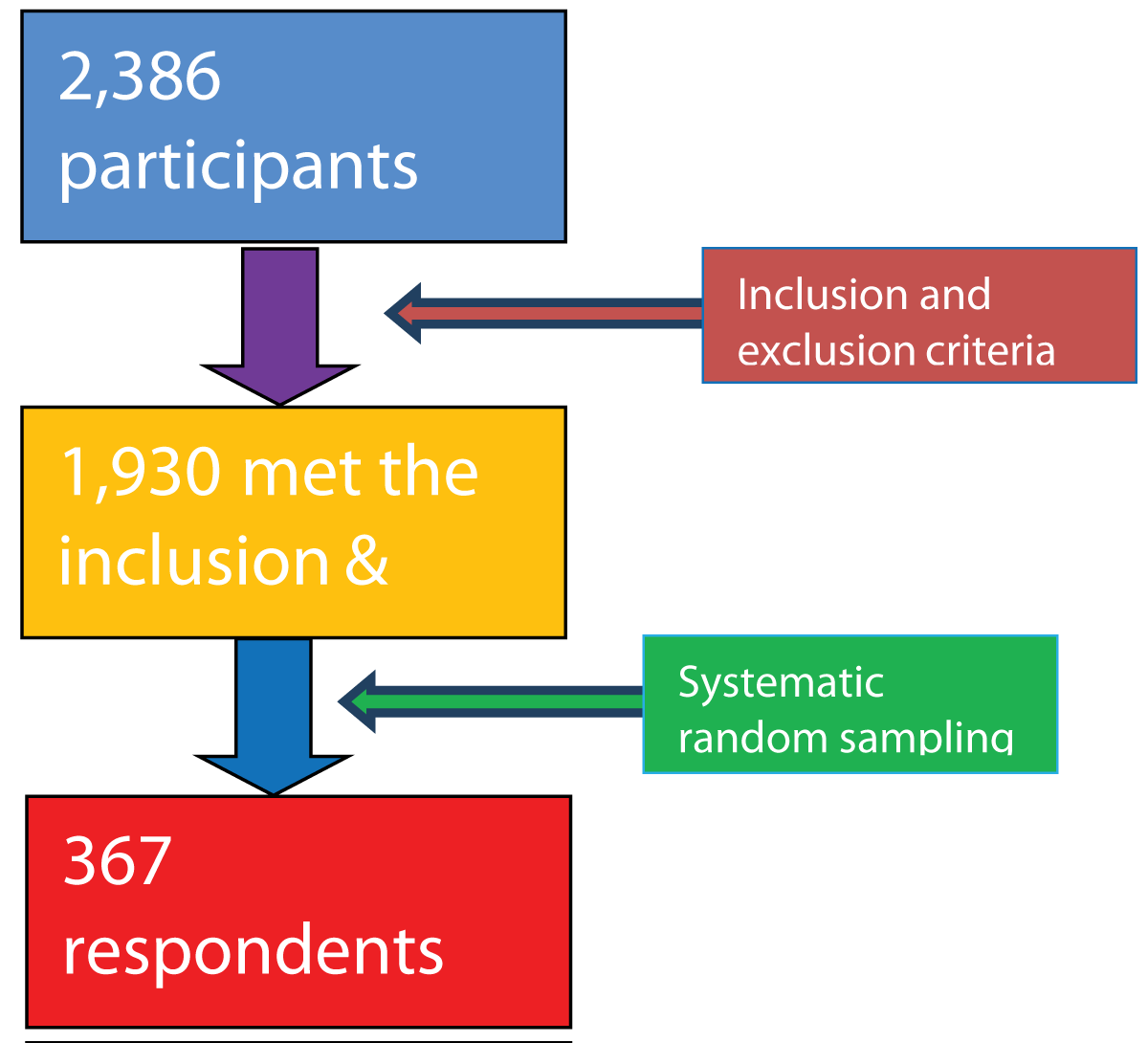
A sampling frame was built, by sorting out the case files of hypertensive patients attending the clinic for the day (Figure 1).
Figure 1: Study flowchart.
Participants who met the inclusion and exclusion criteria on each clinic day were assigned numbers from 1 up to the last number for the day.
The sampling interval (K) was calculated using the formula [19]:
K = N/n
(Where: N = total number of patients, n = calculated minimum sample size and K = sampling interval) [19].
Hence K = 1930/367 = 5.26 which is approximately 5.
A systematic random sampling technique was then used to select the participants on each clinic day; hence, every 6th consenting hypertensive patient who met the inclusion criteria was enrolled for this research. Therefore, an average of five (5) hypertensive patients was recruited per day.
To ensure that a patient was not selected twice, a register for all patients that participated in the study was opened, using their hospital numbers and a colour tag on their file jackets.
Inclusion criteria
1. All consenting adult hypertensive patients aged 18 years and above.
2. Patients who have been diagnosed and on treatments for hypertension for at least 3 months in the clinic and had recorded a minimum of three (3) consecutive clinic visits in the last six months before recruitment to ensure familiarity with diagnosis and prescribed treatment modalities.
Exclusion criteria
1. Patients with co-morbidity (Chronic Kidney Disease, Diabetes)
2. Critically ill patient as at the time of the study (Hypertensive emergency, Congestive cardiac failure, Cerebrovascular accident).
3. Pregnant hypertensive patients belong entirely to another class of hypertension.
Data collection and instruments
Socio-demographic variables were obtained using a semi-structured interviewer-administered questionnaire Clinical parameters (including BP) of respondents were measured, recorded, and graded by the researcher.
Assessment of patients’ level of Spirituality was done using the Spiritual perspective scale (SPS). It is a 10-item tool designed to measure the extent to which individuals hold certain spiritual beliefs and engage in spiritually related behaviors [21,22]. It was scored using the mean [21,22]. The mean spirituality score for this study was 40.9 ± 15.2. The scoring and determination of the level of spirituality are found below (section 3.9.3.3.1) [23]. Scores within 10-35 indicated a low level of spirituality and those ranging between 36-60 indicated a high level of spirituality. Using Cronbach’s alpha, reliability has consistently been rated above 0.90 and average inter-item correlations are 0.878 [8,16,22]. The SPS has been used successfully in prior African studies [9,23].
Scoring and determination of the level of spirituality
Ten items are measuring the beliefs and behaviors of respondents on a 6-point Likert scale [21,22].
The minimum and maximum obtainable scores were 10 and 60 respectively.
Range = minimum possible score – maximum possible score.
Number of expected outcomes = Respondents’ level of spirituality dichotomized into high or low. i.e. 2 divisions
For this study, respondents’ level of spirituality is dichotomized into high or low.
This gives a range of 60-10 = 50
Interval = Range (50)
The number of expected outcomes (2). Interval is 25
Therefore
10 to 35 (minimum score + interval) is a low level of spirituality
36 to 60 is a high level of spirituality
Assessment of Blood Pressure was measured with an Accoson® brand mercury sphygmomanometer.
For this study, a cut-off level of both < 140 mmHg and < 90 mmHg for SBP and DBP respectively were considered Controlled BP. Uncontrolled BP was considered when the SBP and DBP were ≥ 140 mmHg and ≥ 90mmHg respectively using the recommendation of Eight Reports of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-VIII) criteria [24].
Data analysis
All data collected were analyzed using the Statistical Package for Social Sciences (SPSS) for Windows software version 20 (SPSS Inc., Chicago, IL, USA) [25]. The data were presented in tabular form, graphs, and charts as appropriate. Frequency tables and charts were generated for relevant variables. Means, standard deviations, and percentages were determined as appropriate. The means, median, and standard deviation were calculated for continuous variables while categorical variables were analyzed using proportions. The Pearson’s chi-square test was used to assess the bivariate association between spirituality with the respondents’ socio-demographic characteristics and blood pressure control and the Fisher’s exact test was used in analyzing variables with cells less than 5 counts. Binary logistic regression analysis was used to assess the association between the independent variable (spirituality) and dependent variable (blood pressure control) while adjusting for the socio-demographic characteristics. A p - value of equal or less than 0.05 was taken to be statistically significant.
Ethical clearance and consent
Ethical approval was obtained from the Ethics and Research Committee of Federal Teaching Hospital, Ido-Ekiti (Protocol Number: ERC/2016/02/25/08A). Informed verbal consent was obtained from the willing participants. To maintain confidentiality, no names appeared on the questionnaires, but only numbers were used as identifiers. The reporting of this study conforms to the strengthening of the Reporting of Observational Studies in Epidemiology (STROBE) statement [26]. All patients’ details have been de-identified.
Characteristics of respondents
A total of 367 respondents participated in the study. The respondent’s ages ranged between 18 and 82 years, their mean age was 61.1 ± 11.1 years and the majority (58.0%) were older adults (65-82 years). The majority of respondents were female (53.7%) and were married (76.0%), Christians (78.7%), and rural dwellers (64.6%) from the Yoruba tribe (74.7%). Most respondents were traders (37.6%) who had a primary level of education (31.9%) and earned incomes below the poverty line (57.8%). The details of the respondent’s socio-demographic characteristics are shown in Table 1.
| Table 1: Socio-demographic Characteristics of Respondents. | ||
| Variable | Frequency (n = 367) | Percentage (%) |
| Age (years) | 61.1 ± 11.1 | |
| Young Adult (18-35) | 7 | 2.0 |
| Middle-Aged Adult (36-64) | 147 | 40.0 |
| Older Adult (65-82) | 213 | 58.0 |
| Sex | ||
| Male | 170 | 46.3 |
| Female | 197 | 53.7 |
| Marital Status | ||
| Single | 12 | 3.3 |
| Married | 279 | 76.0 |
| Divorced/Separated | 52 | 14.2 |
| Widowed | 24 | 6.5 |
| Religion | ||
| Christianity | 289 | 78.7 |
| Islam | 71 | 19.3 |
| Traditionalist | 7 | 2.0 |
| Domicile | ||
| Urban | 130 | 35.4 |
| Rural | 237 | 64.6 |
| Ethnicity | ||
| Yoruba | 274 | 74.7 |
| Igbo | 55 | 15.0 |
| Hausa | 32 | 8.7 |
| Others | 6 | 1.6 |
| Educational Level | ||
| None | 46 | 12.5 |
| Primary | 117 | 31.9 |
| Secondary | 76 | 20.7 |
| Tertiary | 106 | 28.9 |
| Post Graduate | 22 | 6.0 |
| Occupation | ||
| Professionals | 73 | 19,9 |
| Trading | 138 | 37.6 |
| Farming | 81 | 22.1 |
| Retiree | 39 | 10.6 |
| Self – Employed | 36 | 9.8 |
| Income* | ||
| < Poverty Line (< ₦20,520) | 212 | 57.8 |
| ≥ Poverty Line (≥ ₦20,520) | 155 | 42.2 |
| ₦20,520 is the expected minimum income per month equivalent to $1.90 per day at $1 equals ₦360 (as of July 5, 2017) [41] | ||
Table 2 shows the Spiritual perspective scale based on the spiritual behaviors and beliefs of respondents. Spiritual behaviors that contributed significantly to the high level of spirituality in this study were: private prayers/meditations (χ2 = 3.42, SD = 0.97) and spiritual discussions with family and friends (χ2 = 3.19, SD = 0.92), while Spiritual beliefs that contributed significantly to the high level of spirituality in this study were: forgiveness (χ2 = 3.27, SD = 0.74), seeking spiritual guidance before making decisions (χ2 = 3.26, SD = 0.87) and regarding spirituality as a means of finding live meaning and solving life’s puzzle (χ2 = 3.26, SD = 0.64).
| Table 2a: Spiritual Perspective Scale. | ||||||||||
| S/N | SPS (Spiritual Behaviours) | Not at all | Less than once a year | About once a year | About once a month | About once a week | About once a day | ∑ F | Mean | Standard Deviation |
| 1 | In talking with family and friends, how often do you mention spirituality? | 5 | 12 | 19 | 42 | 123 | 166 | 367 | 3.19 | 0.92 |
| 2 | How often do you share with others the problems and joys of living according to your spiritual beliefs? | 12 | 13 | 12 | 65 | 123 | 142 | 367 | 3.08 | 1.10 |
| 3 | How often do you read spiritually-related material? | 17 | 18 | 24 | 60 | 111 | 137 | 367 | 2.95 | 1.11 |
| 4 | How often do you engage in private prayer and meditation? | 11 | 12 | 7 | 43 | 58 | 236 | 367 | 3.42 | 0.97 |
| Table 2b: Spiritual Perspective Scale. | ||||||||||
| S/N | SPS (Spiritual Beliefs) | Strongly Disagree | Disagree | Disagree more than agree | Agree more than disagree | Agree | Strongly Agree | ∑F | Mean |
Standard Deviation |
| 5 | Forgiveness is an important part of my spirituality. | 6 | 9 | 12 | 13 | 186 | 141 | 367 | 3.27 | 0.74 |
| 6 | I seek spiritual guidance in making decisions in my everyday life. | 6 | 23 | 24 | 29 | 153 | 132 | 367 | 3.26 | 0.87 |
| 7 | My spirituality is a significant part of my life. | 6 | 23 | 33 | 37 | 145 | 123 | 367 | 3.25 | 0.88 |
| 8 | I frequently feel very close to God or a “higher power” in prayer, during public worship, or at important moments in my daily life. | 2 | 23 | 39 | 23 | 159 | 121 | 367 | 3.24 | 0.80 |
| 9 | My spiritual views have had an influence upon influenced my life. | 6 | 12 | 40 | 30 | 157 | 122 | 367 | 3.30 | 0.77 |
| 10 | My spirituality is especially important to me because it answers many questions about the meaning of life. | 2 | 8 | 25 | 38 | 182 | 112 | 367 | 3.26 | 0.64 |
Table 3 shows the level of spirituality among the respondents. More than half (52.6%) of the respondents had a high level of spirituality while 47.4% had a low level of spirituality. The mean spirituality score obtained was 40.9 ± 15.2.
| Table 3: Assessment of the Level of Spirituality among the Respondents. | ||
| Variable | Frequency n = 367 | Percentage (%) |
| Spirituality Perspective Scale | ||
| Low (10-35) | 174 | 47.4 |
| High (36-60) | 193 | 52.6 |
| Total | 367 | 100.0 |
| Mean Spirituality Score ± SD | 40.9 ± 15.2 | |
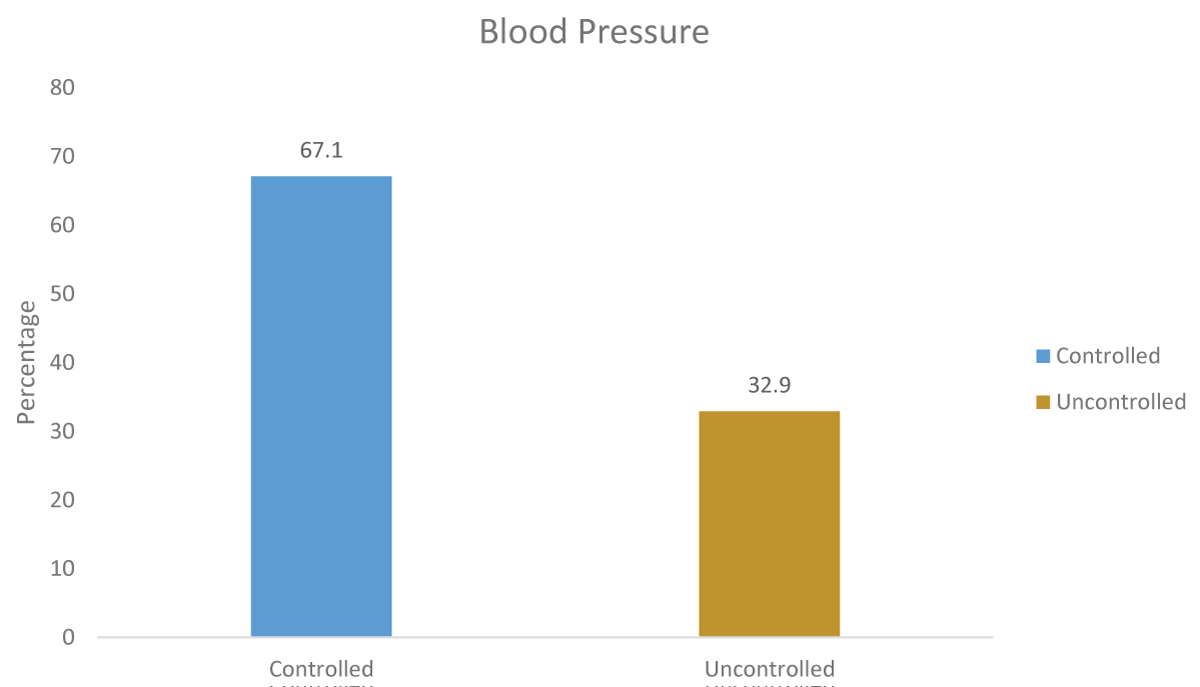
Figure 2 A bar chart showing the level of blood pressure control among the respondents. More than two-thirds (67.1%) of the respondents had controlled blood pressure while 32.9% had uncontrolled blood pressure
Figure 2: A graphical representation of the level of Blood Pressure Control among Respondents.
Table 4 shows the relationship between spirituality and blood pressure among the respondents. It showed that Blood pressure control improves with increasing spirituality. More than two-thirds (69.9%) of those with a high level of spirituality also had good blood pressure control. The relationship was statistically significant as p < 0.05.
| Table 4: Relationships between Blood Pressure Control and Spirituality among the Respondents. | |||||
| Spirituality | |||||
| Variable | Low (10-35) (%) n = 174 |
High (36-60) (%) n = 193 |
Total N=367 |
χ2 | p - value |
| Blood Pressure Control | |||||
| Uncontrolled (≥140/90 mmHg) | 100 (82.6) | 21 (17.4) | 121 (100) | 75.88 | < 0.001 |
| Controlled (< 140/90 mmHg) | 74 (30.1) | 172 (69.9) | 246 (100) | ||
Table 5 shows the relationships between the socio-demographic characteristics of respondents and their level of spirituality. Older adult (64.5%), female (67.5%), married (58.4%), Christian (56.4%), Yoruba (62.8%) and urban dwelling (55.1%) respondents had high levels of spirituality. Also, respondents that had a tertiary level of education (70.8%) who are retired (61.5%), and earned below the poverty line (75.4%) had a high level of spirituality. All variables were statistically significant with p < 0.05 except the area of domicile.
| Table 5: Relationships between the Level of Spirituality and Sociodemographic Characteristics of Respondents. | |||||
| Spirituality | |||||
| Variable | Low (%) n = 174 |
High (%) n = 193 |
Total N = 367 |
χ2 | p - value |
| Age (years) | |||||
| Young Adult (18-35) |
5 (71.4) | 2 (28.6) | 7 (100) | 0.004‡ | |
| Middle-Aged Adult (36-64) | 93 (63.7) | 53 (36.3) | 146 (100) | ||
| Older Adult (65-82) | 76 (35.5) | 138(64.5) | 214 (100) | ||
| Sex | |||||
| Male | 110 (64.7) | 60 (35.3) | 170 (100) | 31.09 | < 0.001 |
| Female | 64 (32.5) | 133 (67.5) | 197 (100) | ||
| Marital Status | |||||
| Single | 12 (100.0) | 0 (0.0) | 12 (100) | 0.001‡ | |
| Married | 116 (41.6) | 163 (58.4) | 279 (100) | ||
| Divorced | 18 (75.0) | 6 (25.0) | 24 (100) | ||
| Separated | 17 (60.7) | 11 (39.3) | 28 (100) | ||
| Widowed | 11 (45.8) | 13 (54.2) | 24 (100) | ||
| Religion | |||||
| Christianity | 126 (43.6) | 163 (56.4) | 289 (100) | 0.018‡ | |
| Islam | 45 (62.5) | 27 (37.5) | 72 (100) | ||
| Traditionalist | 5 (71.4) | 2 (28.6) | 7 (100) | ||
| Domicile | |||||
| Urban | 106 (44.9) | 130 (55.1) | 236 (100) | 1.35 | 0.245 |
| Rural | 68 (51.9) | 63 (48.1) | 131 (100) | ||
| Ethnicity | |||||
| Yoruba | 102 (37.2) | 172 (62.8) | 274 (100) | < 0.001‡ | |
| Igbo | 47 (85.5) | 8 (14.5) | 55 (100) | ||
| Hausa | 22 (68.8) | 10 (31.2) | 32 (100) | ||
| Others | 4 (66.7) | 2 (33.3) | 6 (100) | ||
| Educational Status | |||||
| None | 29 (63.0) | 17 (37.0) | 46 (100) | 21.57 | < 0.001 |
| Primary | 69 (59.0) | 48 (41.0) | 117 (100) | ||
| Secondary | 37 (48.7) | 39 (51.3) | 76 (100) | ||
| Tertiary | 31 (29.2) | 75 (70.8) | 106 (100) | ||
| Post Graduate | 7 (33.3) | 14 (66.7) | 21 (100) | ||
| Occupation | |||||
| Professionals | 35 (43.8) | 45 (56.2) | 80 (100) | 13.43 | 0.009 |
| Trading | 71 (47.7) | 78 (52.3) | 149 (100) | ||
| Farming | 63 (68.5) | 29 (31.5) | 92 (100) | ||
| Self Employed | 27 (61.4) | 17 (38.6) | 44 (100) | ||
| Retired | 15 (38.5) | 24 (61.5) | 39 (100) | ||
| Income | |||||
| < Poverty Line | 52 (24.6) | 159 (75.4) | 211 (100) | 85.96 | < 0.001 |
| ≥ Poverty Line | 122 (78.2) | 34 (21.8) | 156 (100) | ||
| ‡ = Fisher’s Exact Test | |||||
Table 6 explains how some socio-demographic characteristics predicted the level of spirituality. Respondents who were middle-aged adults (1.54 times), Married (7.54 times), Christians (3.38 times), Yoruba (2.23 times), Postgraduate (2.70 times), Professionals (3.54), Less than 5 years on antihypertensive drug (2.72), Controlled blood pressure (4.76 times) and were on 2 drugs or less (2.80 times) were more likely to have a high level of spirituality. However, respondents who were male gender (0.71 times), farmers (0.78), and earned income below the poverty line (0.74 times) were less likely to have high medication adherence.
| Table 6: Logistics Regression for Predictors of Spirituality among the Respondents. | |||||
| Variable | 95% CI | ||||
| OR | Lower | Upper | p - value | ||
| Age group | Young Adult (18-35) | 0.54 | 0.53 | 2.68 | 0.051 |
| Middle-Aged Adult (36-65) | 1.54 | 1.05 | 8.42 | 0.003 | |
| Older Adult (> 65) | 1.0 (RC) | ||||
| Sex | Male | 0.71 | 0.04 | 0.90 | 0.021 |
| Female | 1.0 (RC) | ||||
| Religion | Christianity | 3.38 | 1.22 | 10.81 | 0.004 |
| Islam | 1.11 | 1.08 | 3.29 | 0.031 | |
| Traditionalist | 1.0 (RC) | ||||
| Ethnicity | Yoruba | 2.23 | 1.19 | 9.41 | 0.011 |
| Igbo | 1.53 | 1.04 | 2.92 | 0.016 | |
| Hausa | 1.10 | 0.03 | 3.05 | 0.062 | |
| Others | 1.0 (RC) | ||||
| Education | |||||
| None | 1.0 (RC) | ||||
| Primary | 1.55 | 0.13 | 6.93 | 0.051 | |
| Secondary | 1.11 | 1.04 | 7.42 | 0.012 | |
| Tertiary | 2.13 | 1.67 | 10.54 | 0.037 | |
| Postgraduate | 2.70 | 1.08 | 9.93 | 0.030 | |
| Occupation | |||||
| Professionals | 3.54 | 1.04 | 9.47 | 0.022 | |
| Trading | 1.21 | 1.02 | 6.21 | 0.004 | |
| Farming | 0.78 | 0.09 | 0.99 | 0.016 | |
| Self – Employed | 3.02 | 1.98 | 9.83 | 0.039 | |
| Retired | 1.0 (RC) | ||||
| Income | |||||
| < Poverty Line | 0.74 | 0.10 | 0.97 | 0.006 | |
| > Poverty Line | 1.0 (RC) | ||||
| Blood Pressure | |||||
| Controlled | 4.76 | 1.05 | 14.99 | < 0.001 | |
| Uncontrolled | 1.0 (RC) | ||||
| OR: Odds Ratio; RC: Repeatability Coefficient | |||||
Socio-demographic characteristics of respondents
The socio-demographic profile of the respondents showed that the majority of the respondents were above 65 years. This was higher than reported in a similar hospital-based study in Port-Harcourt by Akpa. et al. [7] and Azinge, et al. in Lagos [27]. It was however lower than the mean age found in an international survey [28]. The reason for the higher preponderance of hypertension in the older age group found in this study compared to other studies might be because this study was done in a rural population as this usually consists of older age groups due to rural-to-urban migration of the young age groups. However, Ido-Ekiti town is a non-industrialized semi-urban setting surrounded by rural settlements.
The majority of the respondents {197 (53.7%)} in this study were females. This aligned with the findings of Iloh, et al. (65.2%) [29] Who also reported a higher prevalence of hypertension in females. It is worthy of note that women are protected from most cardiovascular events compared to men, until after menopause, during which women are at increased risk of cardiovascular complications compared to premenopausal women [30]. Gender differences in blood pressure are inconsistent in many population studies, while some studies quoted a higher prevalence of hypertension among males [30,31], others reported no significant gender difference [32,33]. These inconsistencies could be a result of different age populations or the methodology used in these studies.
In this study about two-thirds {279 (76%)} of all the respondents were married. This was similar to findings by Marfo, et al, [34] who reported 74% married hypertensive patients. However, findings in this study were higher than the 66.4% reported in Ibadan by Ekore, et al. [35]. This difference may be due to the variation in marriage culture in different states and regions among the study populations in Nigeria. Less than a quarter of the population had formal education. This might be due to the study area which is located in the South-Western part of the country where there is a high literacy level which might influence patients’ health-seeking behaviour in terms of them presenting in the hospital for the management of their disease. This study confirms the rating of Ekiti State as an educationally advantaged state. The reported level of literacy was much higher in a hospital-based study done among young adults in Ibadan, South-western Nigeria where about 79.1% of respondents had a minimum of secondary school education [36] and 40.0% reported in Lagos among market women [37]. These differences may be due to the different study populations among whom the studies were conducted.
Level of spirituality among respondents
In Table 3, this study shows that more than half of the respondents had a high level of spirituality. The finding of the majority of the respondents being highly spiritual in this study may not be unconnected with the cultural practices that were inherent in Nigeria. This was similar to a study by Ibraheem, et al. [36] on the relationship between self-reported health status and spirituality among adult patients in Ibadan, Nigeria who found a 51% level of spirituality. In contrast, Jeri and Lynda reported a 100% spirituality level among Nigerians living in America [38]. This is higher than that obtained in the present study, and the difference may be due to the different study populations among whom the studies were conducted and the method used in the study.
In Table 2 Spiritual behaviors that contributed significantly to the high level of spirituality in this study according to Table 3 were private prayers/meditations and spiritual discussions with family and friends. Also, Spiritual beliefs that contributed significantly to the high level of spirituality in this study were forgiveness, seeking spiritual guidance before making decisions, and spirituality as a means of finding meaning to live and solving life’s puzzle.
Relationship between spirituality and blood pressure control
This study shows a significant relationship between spirituality and blood pressure control. This is similar to the finding in a study done on spirituality and blood pressure control by Kretchy, et al. [8] in Umuahia, Nigeria, which showed that participants with a high level of spirituality had a significantly lower diastolic and systolic blood pressure than their counterparts with a low level of spirituality after adjusting for demographic, sociocultural, and psychological variables. High spirituality was found to positively influence the decision by patients to adhere strictly to their antihypertensive medications, therefore, leading to good BP control. However, the findings in this study are higher than what was observed by Quingtao, et al, [39] in a study conducted in China where it was found that 53.4% of those who had a high level of spirituality also had good blood pressure control.
Also, logistic regression shows that for a single unit increase in the level of spirituality, hypertensive patients were almost five times more likely to achieve good blood pressure control. Hence, a high level of spirituality is a significant predictor of good blood pressure control among hypertensive patients.
Relationship between spirituality and sociodemographic characteristics of respondents
In this study, spirituality levels increased with age, and specifically, more than half of the older age group had a higher level of spirituality. This could be a result of the fact that, as people get older, they tend to find solace and meaning in life in the transcendent and hence tend to have more inclination toward spirituality. The above finding is in agreement with hospital-based research conducted by Ibraheem, et al. [36] who also reported an increased level of spirituality with age.
This study established the fact that women have higher spirituality than men. This is possibly due to the vulnerability of women in this part of the world and women tend to find solace in their spiritual practices. This is also similar to what Jeri, et al. [38] found in their study. A higher spirituality score was found among the respondents who were married when compared with the respondents who were single or divorced and this difference was statistically significant. This might be due to the possible encouragement by the spouse towards spirituality, which is not found among the single and the divorced. This trend is in agreement with the finding of Ibraheem, et al. [36] in their study on the relationship between self-reported health status and spirituality among adult patients attending the general outpatient clinic of a tertiary hospital in Ibadan where he reported a higher spirituality level among married people compared with those who were not married [36].
It was observed in this study that spirituality increased with an increase in the level of literacy and this was statistically significant. This might be due to the high literacy level found in a large proportion of the respondents in this study. This is different from the previous finding of Silva, et al. [40] who reported that people of low socio-economic class tend to be more spiritual and that the prevalence of spiritual commitment tends to drop off among higher-income categories.
Recommendations
- Physicians should take appropriate spiritual history while managing patients with hypertension.
- Physicians should encourage their health facilities to have Chaplains and Imams that patients can be referred to for spiritual assistance when needed.
- Physicians should understand their limits by not imposing any form of spiritual practices but rather encourage the practice of what they believe in, in the process of integrating spirituality into their patient’s care.
- Participants with uncontrolled BP should be appropriately referred and encouraged on regular and lifelong use of their antihypertensives to avert devastating vascular complications.
Limitations of the study
1. The study is a cross-sectional study done in a tertiary health institution; the findings may not apply to the general population.
2. Subjects’ ambulatory or home blood pressure readings in out-of-clinic settings were not monitored in this study, and thus the determination of optimal blood pressure control was based on clinic-based measurement alone instead of an average over some time. It is known that the office BP recordings are higher than the home-based recordings. Therefore, those diagnosed with systemic hypertension might have been unnecessarily exposed to antihypertensives with the attendant hypotensive effects and drug intolerance.
3. Spirituality is a dynamic and continuous variable. The dichotomisation in this study represented the levels of spirituality (high or low) at the time of gathering the data. This might not reflect the enduring relationship with a chronic condition like hypertension.
This study has shown that spirituality has a direct influence on blood pressure control among adult hypertensive patients in rural Southwestern, Nigeria. These associations provide direction for future studies that will aid in understanding how health professionals can use this information to provide culturally sensitive and patient-centered care that will improve blood pressure control among patients with hypertension.
The authors would like to appreciate the nurses and resident doctors of the Family Medicine Department and the management of FETHI where the study was conducted.
Funding
The researchers received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Availability of data and materials
The datasets for this study would be made available from the correspondence author on a reasonable request.
Authors’ contribution
1. AO - Conceptualization of the study, designed the study protocol, data acquisition and analysis, and drafted the initial manuscript
2. PO - Literature review, data analysis, and review of manuscript for intellectual content.
3. AOI - Critically revised the protocol for methodological and intellectual content.
All authors have read and approved the final version of the manuscript prior to submission.
- Ogah OS, Okpechi I, Chukwuonye II, Akinyemi JO, Onwubere BJ, Falase AO, Stewart S, Sliwa K. Blood pressure, prevalence of hypertension and hypertension related complications in Nigerian Africans: A review. World J Cardiol. 2012 Dec 26;4(12):327-40. doi: 10.4330/wjc.v4.i12.327. PMID: 23272273; PMCID: PMC3530788.
- Quraishi UM, Begum S, Agarwal A, Chandrasekhar S, Shamji U, Naeem A. A Study to Know the Prevalence and Awareness of Hypertension in Market Population of Ras Al Khaimah, UAE. J Basic Appl Sci Res 2013; 3(2): 458-462.
- Abdullahi AA, Amzat J. Knowledge of hypertension among the staff of University of Ibadan. J Public Health Epidemiol. 2011; 3:204-209.
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC Jr, Svetkey LP, Taler SJ, Townsend RR, Wright JT Jr, Narva AS, Ortiz E. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014 Feb 5;311(5):507-20. doi: 10.1001/jama.2013.284427. Erratum in: JAMA. 2014 May 7;311(17):1809. PMID: 24352797.
- Rao CR, Kamath VG, Shetty A, Kamath A. High blood pressure prevalence and significant correlates: a quantitative analysis from coastal karnataka, India. ISRN Prev Med. 2012 Dec 3;2013:574973. doi: 10.5402/2013/574973. PMID: 24967139; PMCID: PMC4062860.
- World Health Organisation (WHO). Facing the facts: The impact of chronic disease in Nigeria. Geneva: WHO; 2005. Available from: http://www.who.int/chp/chronic disease report/media/nigeria.pdf. Accessed 17th of November 2015.
- Akpa MR, Alasia DD, Emem-Chioma PC. An appraisal of hospital-based blood pressure control in Port Harcourt, Nigeria. The Nigerian Health Journal. 2008; 8(1-2): 27-30.
- Oyati AI, Orogade AA, Danbauchi SS, Azuh PC. Awareness, Treatment and Control of Hypertension among Hypertensives in Zaria. Journal of Medicine in the Tropics. 2011; 13(2): 139-144.
- Kretchy I, Owusu-Daaku F, Danquah S. Spiritual and religious beliefs: do they matter in the medication adherence behaviour of hypertensive patients? Biopsychosoc Med. 2013 Oct 18;7(1):15. doi: 10.1186/1751-0759-7-15. PMID: 24138844; PMCID: PMC3854617.
- Prasad DS, Kabir Z, Dash AK, Das BC. Prevalence and predictors of adult hypertension in an urban eastern Indian population. Heart Asia. 2012 Jan 1;4(1):49-52. doi: 10.1136/heartasia-2011-010071. PMID: 27326028; PMCID: PMC4898618.
- Chagas C, Martins LB, Machado FR, Zangari W, Galduróz JCF. Religious and secular spirituality: Methodological implications of definitions for health research. Explore (NY). 2023 Jan-Feb;19(1):6-13. doi: 10.1016/j.explore.2022.04.004. Epub 2022 Apr 12. PMID: 35469748.
- Koenig HG. Religion, spirituality, and health: The research and clinical implications. International Scholarly Research Notices, 2012.
- Cruz JP, Colet PC, Alquwez N, Inocian EP, Al-Otaibi RS, Islam SM. Influence of religiosity and spiritual coping on health-related quality of life in Saudi haemodialysis patients. Hemodial Int. 2017 Jan;21(1):125-132. doi: 10.1111/hdi.12441. Epub 2016 Jun 21. PMID: 27329681.
- Kent BV, Upenieks L, Kanaya AM, Warner ET, Cozier YC, Daviglus ML, Eliassen H, Jang DY, Shields AE. Religion/Spirituality and Prevalent Hypertension among Ethnic Cohorts in the Study on Stress, Spirituality, and Health. Ann Behav Med. 2023 Jul 19;57(8):649-661. doi: 10.1093/abm/kaad007. PMID: 37265144; PMCID: PMC10354840.
- Buck AC, Williams DR, Musick MA, Sternthal MJ. An examination of the relationship between multiple dimensions of religiosity, blood pressure, and hypertension. Soc Sci Med. 2009 Jan;68(2):314-22. doi: 10.1016/j.socscimed.2008.10.010. Epub 2008 Nov 18. PMID: 19019516; PMCID: PMC2654362.
- Kharitonov SA. Religious and Spiritual Biomarkers in both Health and Disease. Religions. 2012; 3(2):467-497.
- Kreikebaum S, Guarneri E, Talavera G, Madanat H, Smith T. Evaluation of a holistic cardiac rehabilitation in the reduction of biopsychosocial risk factors among patients with coronary heart disease. Psychol Health Med. 2011 May;16(3):276-90. doi: 10.1080/13548506.2010.542170. PMID: 21491336.
- Holt-Lunstad J, Steffen PR, Sandberg J, Jensen B. Understanding the connection between spiritual well-being and physical health: an examination of ambulatory blood pressure, inflammation, blood lipids and fasting glucose. J Behav Med. 2011 Dec;34(6):477-88. doi: 10.1007/s10865-011-9343-7. Epub 2011 Apr 13. PMID: 21487720.
- Araoye MO. Sample size determination. Research Methodology with Statistics for Health and Social Sciences, Ilorin: Nathadex Publishers. 2004; 115-121.
- Ayogu RNB, Ezeh MG, Okafor AM. Prevalence and predictors of different patterns of hypertension among adults aged 20-60 years in rural communities of Southeast Nigeria: a cross-sectional study. Arch Public Health. 2021 Nov 25;79(1):210. doi: 10.1186/s13690-021-00724-y. PMID: 34819152; PMCID: PMC8613986.
- Reed PG. Spirituality and well-being in terminally ill hospitalized adults. Res Nurs Health. 1987 Oct;10(5):335-44. doi: 10.1002/nur.4770100507. PMID: 3671781.
- Kim SS, Reed PG, Kang Y, Oh J. Translation and psychometric testing of the Korean Versions of the Spiritual Perspective Scale and the Self-transcendence Scale in Korean elders. J Korean Acad Nurs. 2012 Dec;42(7):974-83. doi: 10.4040/jkan.2012.42.7.974. PMID: 23377593.
- Dailey DE, Stewart AL. Psychometric characteristics of the spiritual perspective scale in pregnant African-American women. Res Nurs Health. 2007 Feb;30(1):61-71. doi: 10.1002/nur.20173. PMID: 17243108.
- Gee ME, Campbell N, Sarrafzadegan N, Jafar T, Khalsa TK, Mangat B, Poulter N, Prabhakaran D, Sonkodi S, Whelton PK, Woodward M, Zhang XH. Standards for the uniform reporting of hypertension in adults using population survey data: recommendations from the World Hypertension League Expert Committee. J Clin Hypertens (Greenwich). 2014 Nov;16(11):773-81. doi: 10.1111/jch.12387. Epub 2014 Aug 26. PMID: 25157607; PMCID: PMC8031637.
- SPSS Inc. Predictive Analytics Software Statistics for Windows, Version 20.0. Chicago: SPSS Inc. 2009.
- von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007 Oct 16;147(8):573-7. doi: 10.7326/0003-4819-147-8-200710160-00010. Erratum in: Ann Intern Med. 2008 Jan 15;148(2):168. PMID: 17938396.
- Azinge EC, Sofola OA, Silva BO. Relationship between salt intake, salt-taste threshold and blood pressure in Nigerians. West Afr J Med. 2011 Sep-Oct;30(5):373-6. PMID: 22752827.
- Thoenes M, Bramlage P, Zhong S, Shang S, Volpe M, Spirk D. Hypertension control and cardiometabolic risk: a regional perspective. Cardiol Res Pract. 2012;2012:925046. doi: 10.1155/2012/925046. Epub 2012 Jan 2. PMID: 22242212; PMCID: PMC3254169.
- Iloh GU, Amadi AN, Okafor GO, Ikwudinma AO, Odu FU, Godswill-Uko EU. Adherence to lifestyle modifications among adult hypertensive Nigerians with essential hypertension in a primary care clinic of a tertiary hospital in resource-poor environment of Eastern Nigeria. British Journal of Medicine and Medical Research. 2014; 4(18):3478-3490.
- Shaw BH, Protheroe CL. Sex, drugs and blood pressure control: the impact of age and gender on sympathetic regulation of arterial pressure. J Physiol. 2012 Jun 15;590(12):2841-3. doi: 10.1113/jphysiol.2012.229237. PMID: 22707595; PMCID: PMC3448151.
- Maranon R, Reckelhoff JF. Sex and gender differences in control of blood pressure. Clin Sci (Lond). 2013 Oct;125(7):311-8. doi: 10.1042/CS20130140. PMID: 23746374; PMCID: PMC4283814.
- Sarganas G, Neuhauser HK. The persisting gender gap in hypertension management and control in Germany: 1998 and 2008-2011. Hypertens Res. 2016 Jun;39(6):457-66. doi: 10.1038/hr.2016.5. Epub 2016 Jan 28. PMID: 26818655.
- Podpalov V, Scahstlivenko A, Zhurova V, Deev A, Ogrisko N, Vakar D, Podpalov VV. Gender difference in hypertension prevalence and cardiovascular risk factors in a Belarus urban population: 2010; 7: 304.
- Marfo AFA, Owusu-Daaku FT, Addo MO, Saana II. Ghanaian hypertensive patients understanding of their medicines and life style modification for managing hypertension. Int J Pharm Pharm Sci. 2014; 6(4): 165-170.
- Ekore RI, Ajayi IO, Arije A. Case finding for hypertension in young adult patients attending a missionary hospital in Nigeria. Afr Health Sci. 2009 Sep;9(3):193-9. PMID: 20589150; PMCID: PMC2887025.
- Ibraheem AB, Ibraheem WA, Adebusoye L. The relationship between self-reported health status and spirituality among adult patients attending general outpatient clinic of tertiary hospital in ibadan. Ann Ib Postgrad Med. 2014 Jun;12(1):31-7. PMID: 25332698; PMCID: PMC4201931.
- Busari A, Olayemi S, Oreagba I, Alabidun A. Educational intervention as a strategy for improving blood pressure status of market women in Lagos, Nigeria. The Internet Journal of Health. 2010; 11(1):771-777.
- Jeri D, Linda LD. Spiritual perspectives and health: A random survey in a Southern State. Online J Rural Nurs Health Care. 2009; 9(2):23-31.
- Meng Q, Xu Y, Shi R, Zhang X, Wang S, Liu K, Chen X. Effect of religion on hypertension in adult Buddhists and residents in China: A cross-sectional study. Sci Rep. 2018 May 29;8(1):8203. doi: 10.1038/s41598-018-26638-4. PMID: 29844414; PMCID: PMC5974409.
- Silva CF, Borges FR, Avelino CCV, Miarelli AC, Vieira GA, Goyata ST. Spirituality and Religiosity in patients with systemic arterial hypertension. Rev bioet (impr). 2016; 24(2):332-343.
- Poverty. Data. Data.worldbank.org. 2017. http://data.worldbank.org/topic/poverty#.